Neonatal Follow-up
NICU Follow Up and Neurodevelopmental 2: Neonatal Growth, Nutrition and the Brain
205 - Maternal pre-pregnancy obesity and sex-specific associations with neonatal brain volumes in regions that modulate cognition and behavior
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 205
Publication Number: 205.144
Publication Number: 205.144
Carmen Monthe-Dreze, Brigham and Women's Hospital, Boston, MA, United States; Sarbattama Sen, Brigham and Women’s Hospital, Boston, MA, United States; Patricia Ellen Grant, Boston Children's Hospital, Boston, MA, United States; Laura Holsen, Harvard Medical School, Boston, MA, United States; Tara Smyser, Washington University in St. Louis, St. Louis, MO, United States; Terrie Inder, Childrens Hospital of Orange County, Irvine, CA, United States; Sarah K. England, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Cynthia Rogers, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Deanna Barch, Washington University in St. Louis School of Medicine, Saint louis, MO, United States; Barbara Warner, Division of Newborn Medicine, St Louis, MO, United States; Joan Luby, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Christopher D. Smyser, Washington University in St. Louis, St. Louis, MO, United States

Carmen Monthe-Dreze, MD (she/her/hers)
Neonatologist/Instructor in Pediatrics
Brigham and Women's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Children exposed to maternal obesity (MatOb) in utero are more likely to have executive dysfunction and emotional dysregulation. Animal models of MatOb suggest that these effects may be mediated by sex-dependent disrupted brain architecture. However, little is known on the sex-specific impact of pre-pregnancy obesity on fetal brain development in regions supporting attention and regulatory control in humans.
Objective: Determine associations of MatOb with neonatal brain volumetrics and whether associations differ by sex.
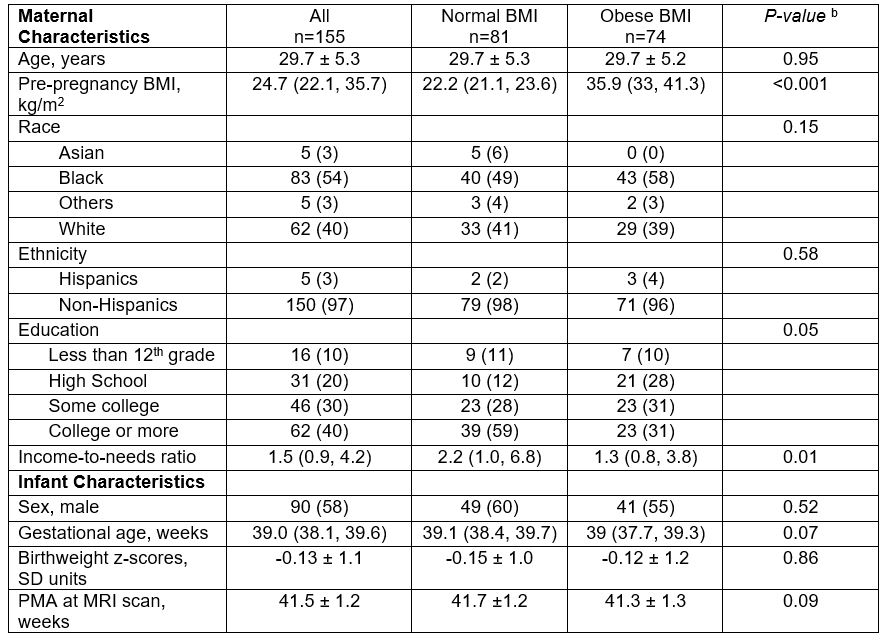
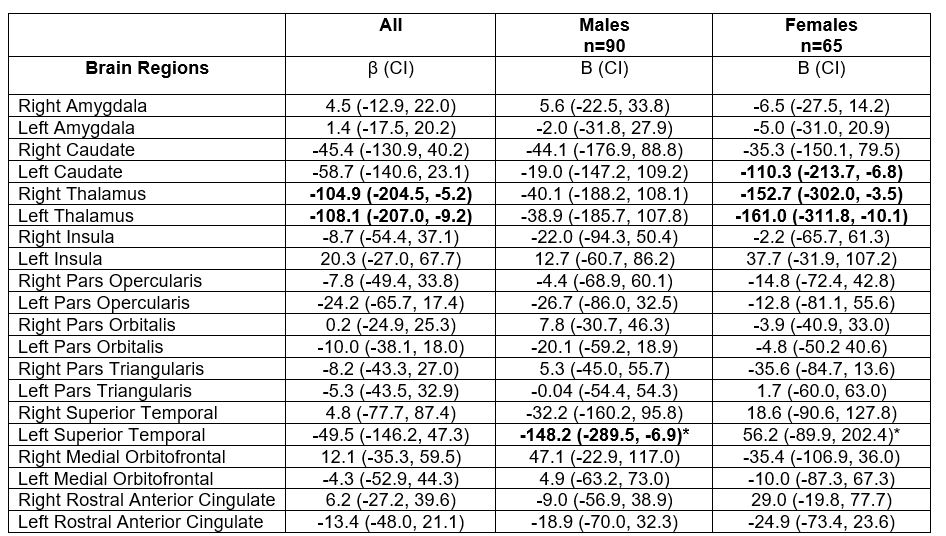
Design/Methods: Subjects were from a longitudinal pre-birth cohort study (Early Life Adversity and Biologic Embedding) of mothers and their term infants who underwent brain magnetic resonance imaging (MRI). The exposure was pre-pregnancy body mass index (BMI) category (MatOb: BMI ≥ 30 vs. Normal: BMI ≥18.5 and < 25 kg/m2). We used multivariable linear regression to evaluate associations of BMI category with volumetrics in a priori defined brain regions. We evaluated whether associations of BMI category with brain volumetrics differ by infant sex, using BMI*sex interaction terms and stratified models to test the interaction. Confounders included maternal education, race, income-to-needs ratio; infant sex, birthweight-z-score, post-menstrual age at MRI, and intracranial volume.
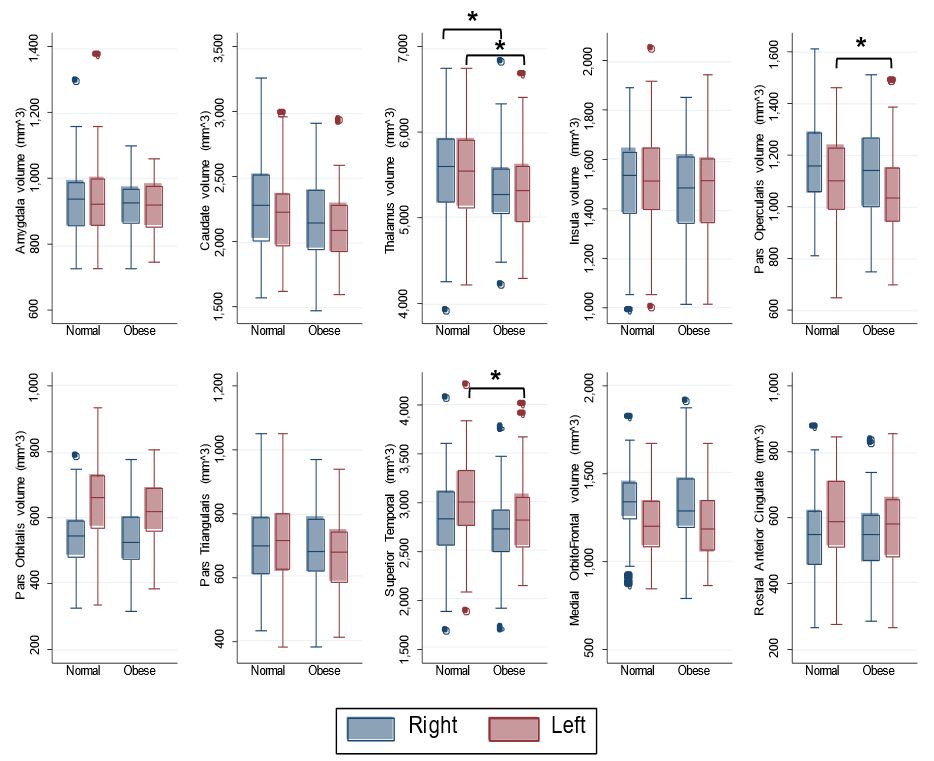
Results: We included 155 mothers (60% non-White, 48% with obesity; mean [SD] age at delivery 29.7 [5.3] y) and their infants (58% male; mean [SD] gestational age 38.9 [1.0] wks, postmenstrual age at MRI 41.5 [1.2] wks, Table 1). In unadjusted analyses, compared to infants of mothers with normal BMI, infants exposed to MatOb in utero had lower volumes in the bilateral thalami, left pars opercularis, and left superior temporal cortex (Figure). In adjusted models, in utero exposure to MatOb was associated with lower bilateral thalami volumes only (Right: β, -104.9 mm3, 95%CI: -204.5, -5.2; Left: -108.1 [-207,-9.2], Table 2). In sex-stratified analyses, MatOb was associated with lower left caudate and bilateral thalami volume in females, but not males, though effects size did not significantly differ by sex (P-int >.2); Additionally, exposure to MatOb was associated with lower left superior temporal cortical volume in males (-148.2 [-289.5, -6.9]), but not females (56.2, [-89.9, 202.4], P-int=.04).
Conclusion(s): Maternal obesity was associated with lower neonatal brain volumes in a sex-specific manner in regions important for executive function, reward valuation, and emotional regulation. These findings provide mechanistic insights in the associations of pre-pregnancy obesity with offspring cognition and behavior.