Neonatal GI Physiology & NEC
Neonatal GI Physiology & NEC 1: GI Health and NEC Complications
326 - Clinical impact of timing of surgery on outcomes in preterm infants with surgical necrotizing enterocolitis
Publication Number: 326.133

Parvesh Mohan Garg, MD (he/him/his)
Associate Professor
Atrium Health Wake Forest Baptist
Winston Salem, North Carolina, United States
Presenting Author(s)
Background: The clinical impact of timing of surgery on outcomes in preterm infants with surgical necrotizing enterocolitis (NEC) are not well defined.
Objective:
We sought to investigate the impact of different timing of surgery from the day of NEC diagnosis on clinical outcomes in preterm infants with surgical NEC.
Design/Methods:
Retrospective comparison of clinical information by the timing of surgery at three different time points (more than versus < 48 hours, 96 hours and 1 week) in preterm infants with surgical NEC. Associations between timing of surgery and clinical factors/outcomes were assessed with univariate and multivariable logistic regression analyses.
Results:
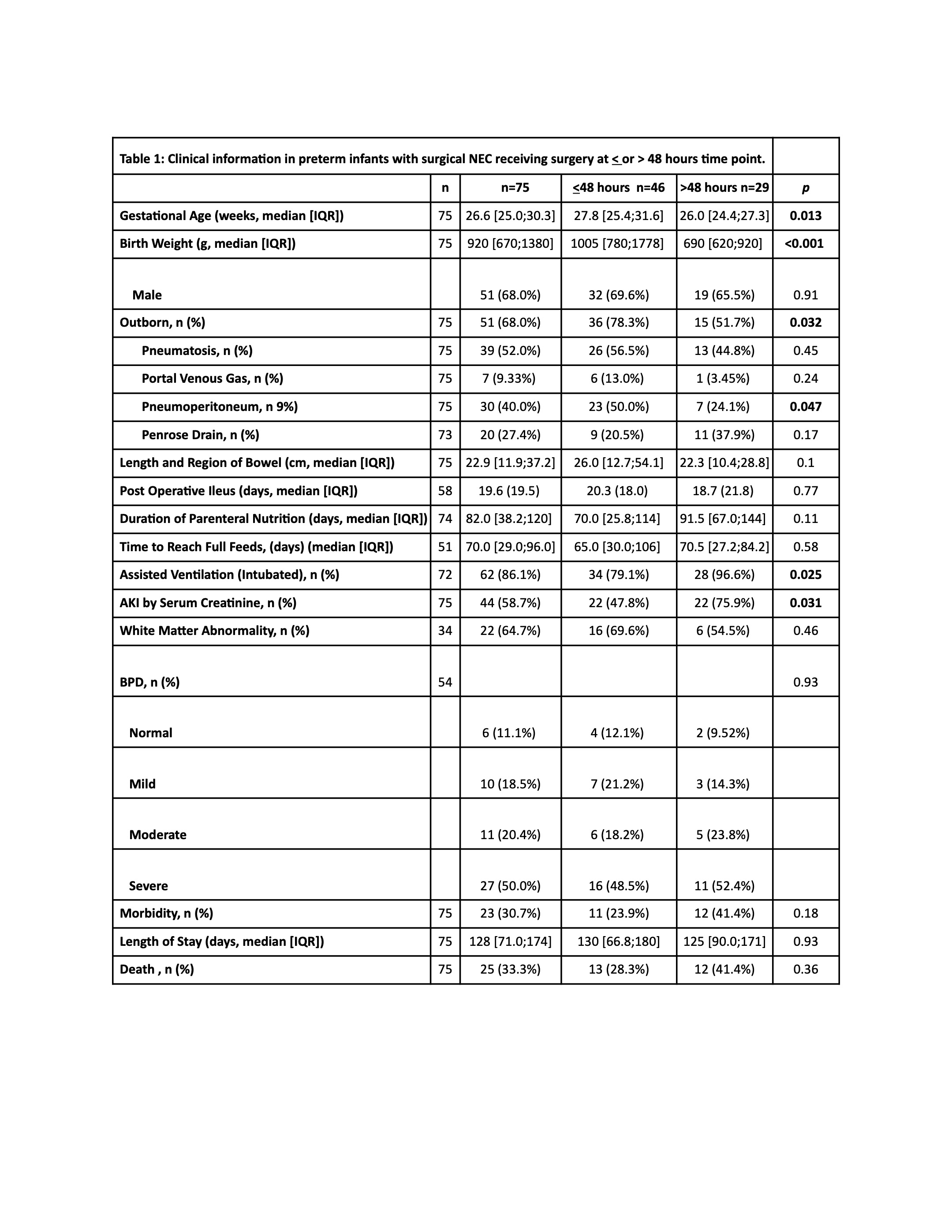
Seventy-five infants were included in the analysis. Those who received surgery after 48 hours (n= 29/75) had lower median gestational age (26 weeks [24.4;27.3] vs 27.8 [25.4;31.6]; p=0.013), lower median birth weight (690 gm [620;920] vs. 1005 gm [780;1778];p=< 0.001), had less pneumoperitoneum, were out born(51.7% vs. 78.3%;p=0.032) less frequently, had higher acute kidney injury (75% vs 47.8% ;p=0.031), were intubated and ventilated ( 96% vs 79% ;p=0.025) more frequently and had higher hemorrhagic lesions (p=0.019) and reparative lesions (28% vs 62%; p=0.008) on histopathology than those receiving surgery before 48 hours (n=46/75) [Table 1].
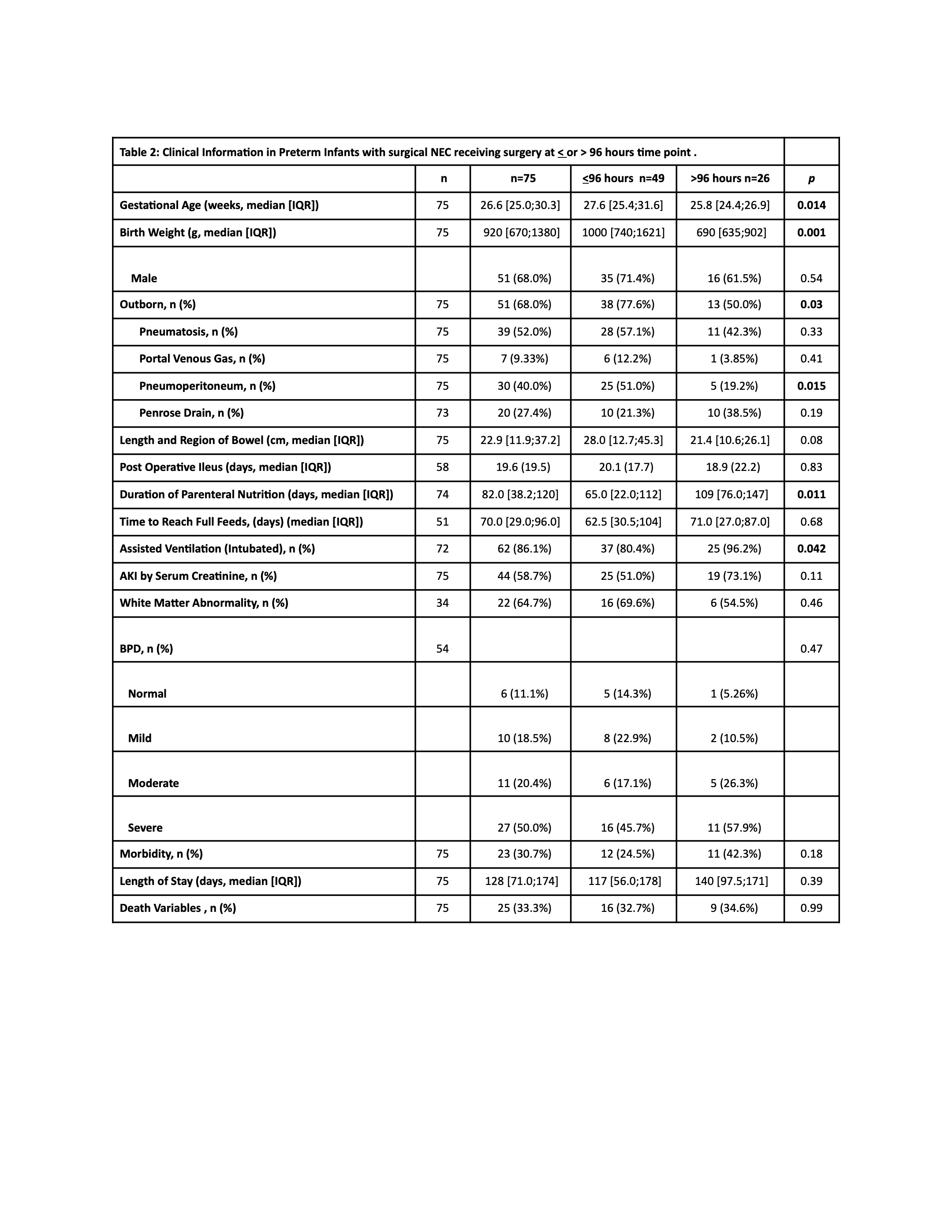
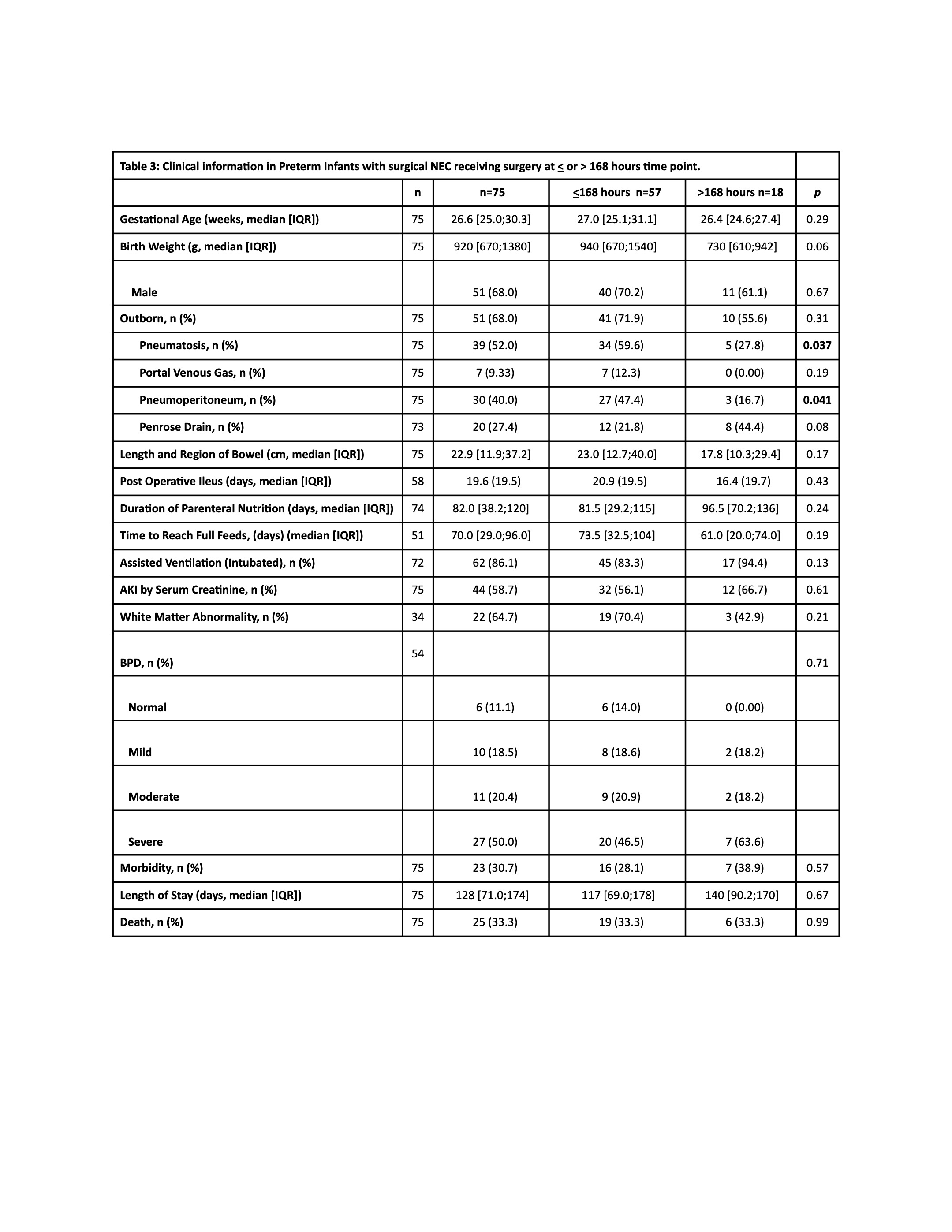
Infants receiving surgery after 96 hours had similar trends except had significantly lower hematocrit and longer parenteral nutrition dependence (109 days [76.0;147] vs 65.0 [22.0;112]; p=0.011) than less than 96 hours group [Table2]. The infants receiving surgery after 1 week had significantly lower birth weight and had higher reparative changes (p=0.026) and cholestasis (89% vs 59%; p=0.04) than those receiving surgery < 1 week [Table3].
There was no significant impact of surgery timing on the length of bowel loss, surgical morbidity, bronchopulmonary dysplasia, white matter injury on brain MRI or mortality.
Conclusion(s):
The infants receiving surgery later were young and smaller and received parenteral nutrition longer with no significant impact on morbidities and mortality.