Adolescent Medicine: General
Adolescent Medicine 1
440 - Changes in Patterns of Diagnosing Sexually Transmitted Infections in Adolescents During COVID-19
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 440
Publication Number: 440.1
Publication Number: 440.1
Lauren Titus, Children's Hospital of Wisconsin, Milwaukee, WI, United States; Kelsey Porada, Medical College of Wisconsin, Milwaukee, WI, United States; Melodee Liegl, Medical College of Wisconsin, Milwaukee, WI, United States; Amy Pan, Medical College of Wisconsin, Milwaukee, WI, United States; Vanessa McFadden, Medical College of Wisconsin, Milwaukee, WI, United States
.jpg)
Lauren Titus, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
Children's Hospital of Wisconsin
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: Adolescents are known to be at high risk for sexually transmitted infections (STIs), with over half (53%) of reported cases in 2020 being among adolescents and young adults aged 15-24 years old. The COVID-19 pandemic led to missed primary care and preventative health visits as well as delays in care for non-urgent complaints. Many areas of routine screening typically performed in primary care settings were deferred, including STI screening. Because of this, hospitals and emergency departments (EDs) may have served as alternative sources for routine health screenings for adolescents, who were often seeking healthcare for a reason unrelated to sexual health or did not have a primary medical home.
Objective: The objective of this study is to determine changes in patterns of STI testing for adolescents in non-traditional settings such as the ED or inpatient setting before & after the COVID-19 pandemic.
Design/Methods: Our team conducted a retrospective review using data from the Public Health Information System (PHIS) database for patients discharged from January 2019 through March 2022. As one of the most commonly obtained tests for STI testing or routine screening, Chlamydia PCR testing was analyzed in our study. The frequency of chlamydia PCR testing pre- and post-March 2020 was compared (including ED vs inpatient setting in the model and treating hospital number as random). Patient characteristics and patient setting (ED v. inpatient setting) were compared using Pearson Chi-square.
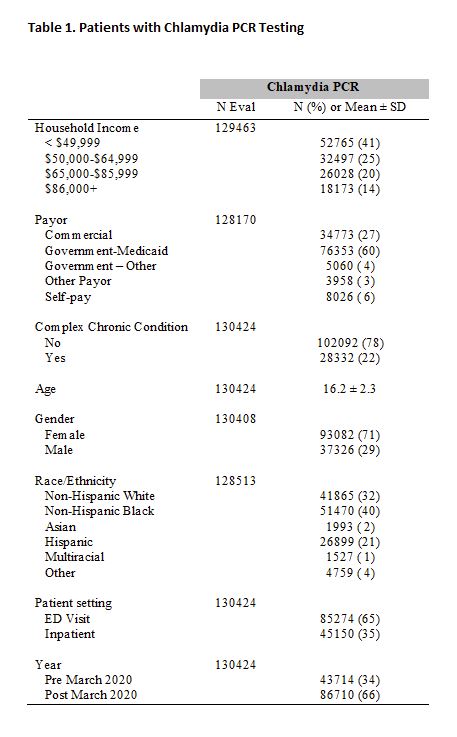
Results: Table 1 highlights that the majority of our study population who were tested were female (71%) without chronic conditions (78%), had < $50,000 for household income (41%), and used government insurance (64%). Mean ± SD age of tested individuals was 16.2 ± 2.3 years. The majority of individuals tested were in the ED context (65%). Chlamydia PCR testing was three times more likely to be done in the pre-pandemic period compared to post-pandemic (OR = 3.15 95% CI 2.90-3.42, p < 0.0001) when patient type was included in the model and hospital was treated as random. Tables 2 and 3 outline the characteristics of patients tested for Chlamydia by year comparing pre- and post-March 2020 and comparing patient setting (ED vs. Inpatient), respectively.
Conclusion(s): Contrary to our hypothesis, chlamydia testing was actually more frequently performed pre-pandemic. Further research should be pursued to determine the reasons behind decreased STI testing and to determine how clinically relevant demographic differences between settings are, despite statistical significance.
.jpg)
.jpg)
