Critical Care
Critical Care 1
2 - Blood Prime-Circuit Interplay Does Not Explain the Inflammogenic Effect of Extracorporeal Membrane Oxygenation in Pediatric Patients
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 2
Publication Number: 2.107
Publication Number: 2.107
Michelle J. Mejia, St. Christopher's Hospital for Children, Haddonfield, NJ, United States; Swosti Joshi, St. Christopher's hospital for children /Drexel University College of Medicine, Philadelphia, PA, United States; Vilmaris Quinones Cardona, St Christopher’s Hospital for Children/Drexel University College of Medicine, Philadelphia, PA, United States; Alison J.. Carey, St. Christopher's Hospital for Children, Philadelphia, PA, United States; Ogechukwu Menkiti, St. Christopher's Hospital for Children, cherry Hill, NJ, United States

Michelle J. Mejia, MD (she/her/hers)
Neonatology Fellow
St. Christopher's Hospital for Children
Haddonfield, New Jersey, United States
Presenting Author(s)
Background: Systemic inflammatory response syndrome (SIRS) in pediatric extracorporeal membrane oxygenation (ECMO) is the result of a complex interplay between the patient's pre-ECMO inflammatory status, immune cell activation by a non-endothelialized circuit, blood prime-circuit interaction, and ongoing exposure to blood products. A better understanding of the inflammatory milieu in pediatric ECMO patients may help target management strategies.
Objective: We hypothesize that the initiation of ECMO increases proinflammatory cytokines in pediatric patients.
Design/Methods: A single-center prospective cohort study of an ex-vivo ECMO circuit model and in-vivo critically ill pediatric patients from 08/2021-07/2022. Subjects were divided into two groups- the medical group, those who responded to maximum medical therapy, and the ECMO group, those refractory to medical management who required ECMO. Serial blood samples were collected at 0,2,4,8,12 and 24-hour time points, and plasma was immediately stored at -80°C until Luminex multiplex bead assay (Luminex, Austin, TX) was performed. In the medical group, sample collection ceased if a subject was cannulated for ECMO or died.
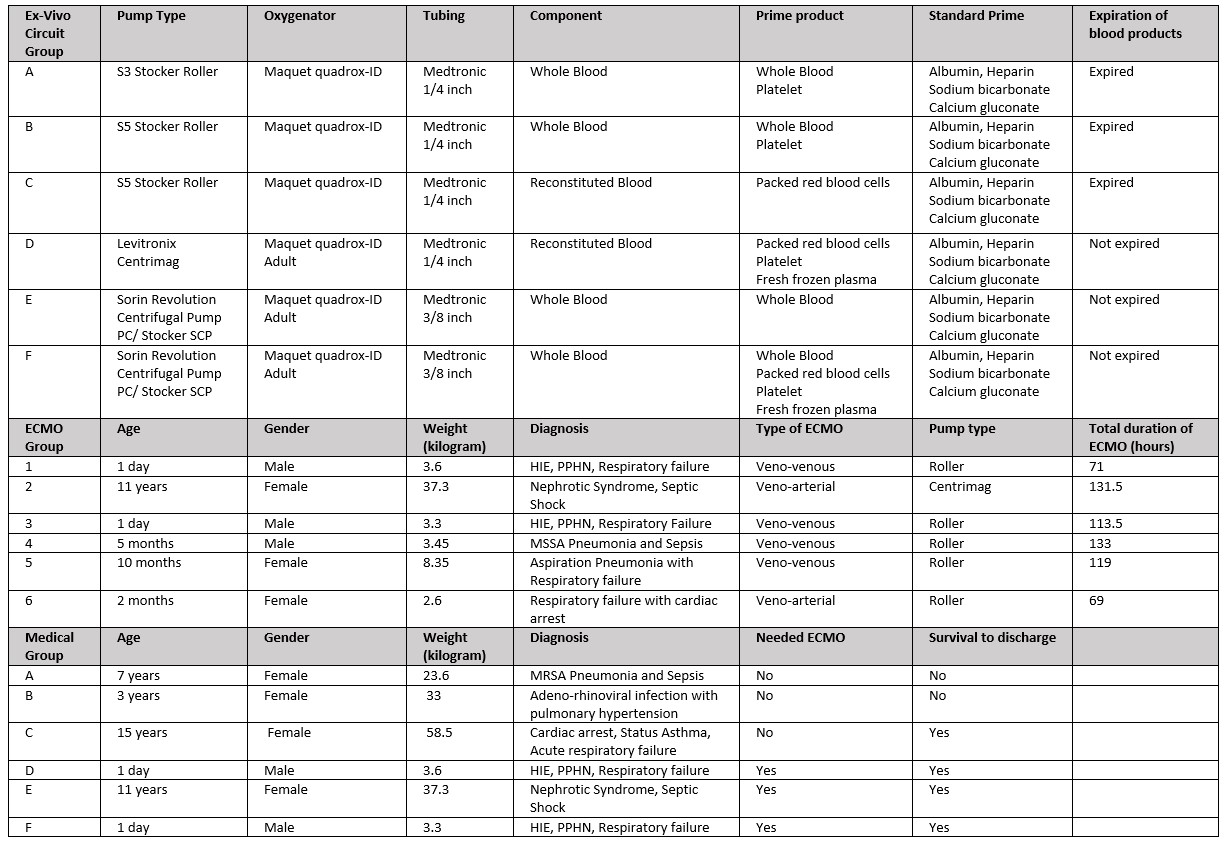
Results: The ex-vivo group comprised six ECMO circuits, of which 67% had whole blood prime and 50% used roller pumps. Nine discrete subjects were enrolled, three solely in the medical group, three with cross-over from the medical to ECMO group, and three solely in the ECMO group. Subjects were mainly female (67%), 0-15 years of age, with respiratory failure (67%). In the ECMO group, 67% were on veno-venous ECMO and median duration of ECMO was 116 hrs. (69-133 hrs.) (Table1).
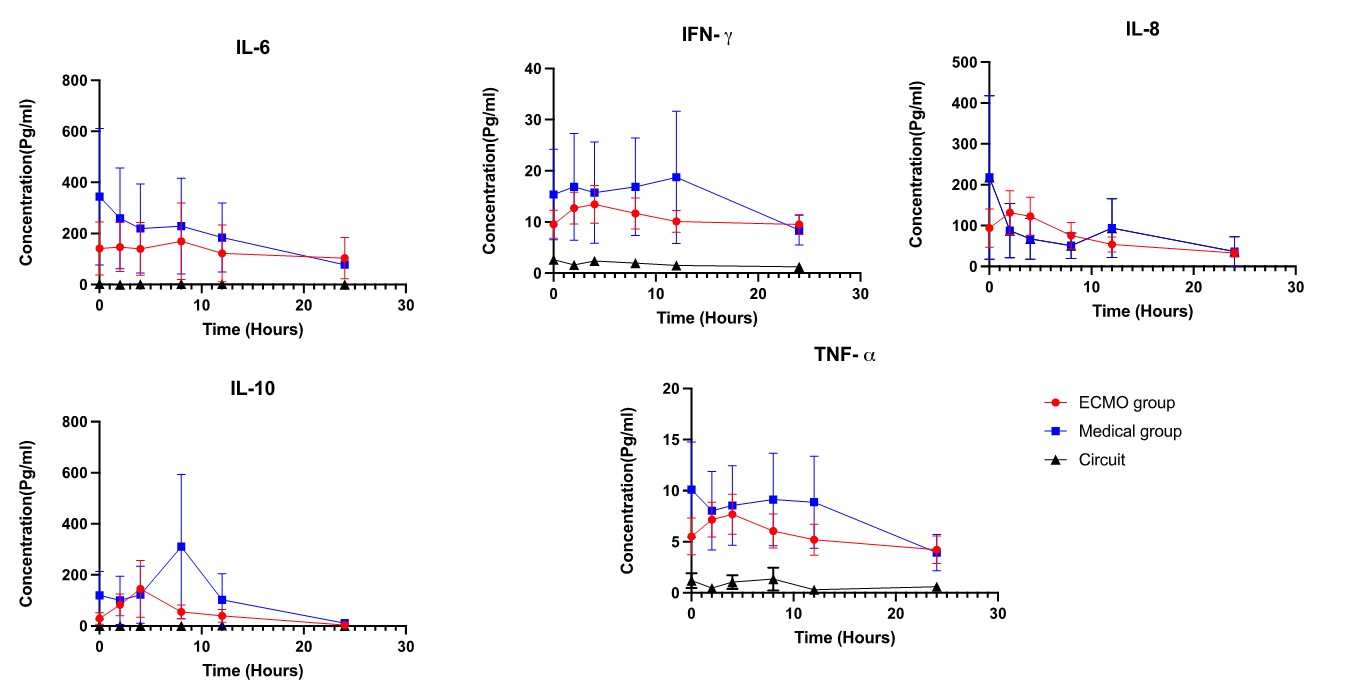
Proinflammatory and anti-inflammatory cytokines- specifically IL-6, IL-8, TNF-∝, IFN-γ, and IL-10- were minimally detected in the ex-vivo circuit. These markers were elevated in both ECMO and medical groups without significant differences (Figure 1). Expected pro-inflammatory cytokines IL-1B and anti-inflammatory cytokines IL-4 and IL-13 were not detected. There was statistically significant increase in macrophage inflammatory proteins (MIP) in ECMO compared to medical group at 2 hrs. for MIP-1b and at 12 hrs. for MIP-3a (Figure 2).
Conclusion(s): Our study suggests the sole interaction between the circuit and blood prime does not significantly contribute to the inflammatory response seen during ECMO initiation. Macrophage inflammatory proteins such as MIP-1b and MIP-3a may play a role in pediatric ECMO-related SIRS. Further studies are needed to investigate the role of these markers.
.jpg)

