Telemedicine/EHR/Medical Informatics
Telemedicine/EHR/Medical Informatics 1
736 - Pediatric Primary Care Management of Overweight/Obesity: the Role of Electronic Health Record Tools
Publication Number: 736.154

Mona Sharifi, MD, MPH (she/her/hers)
Associate Professor of Pediatrics and of Public Health
Yale School of Medicine
New Haven, Connecticut, United States
Presenting Author(s)
Background:
Electronic health record (EHR)-based clinical decision support (CDS) systems can promote guideline adherence. To avoid exacerbating workload burden when implementing CDS, it is critical to understand clinicians’ existing workflows, experiences, and technology acceptance.
Objective:
To describe clinicians’ use of existing and projected acceptance of future EHR-based tools to prepare for a multi-site trial of tailored CDS to support management of overweight/obesity (OW/OB) in heterogenous pediatric primary care settings.
Design/Methods:
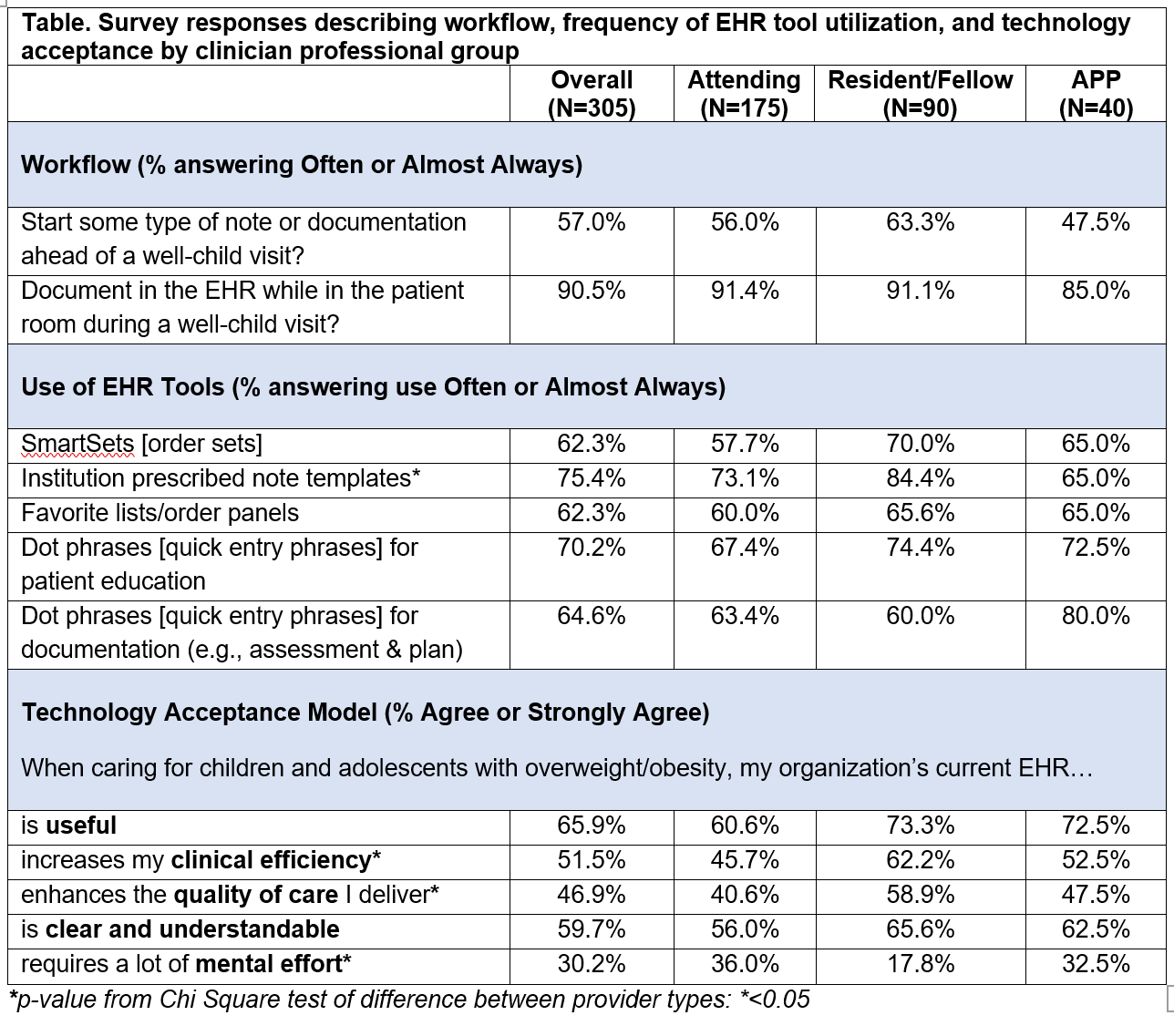
We distributed an online survey to p</span>rimary care clinicians at 79 clinics across three US health systems in the Northeast, South, and Midwest. The survey included Likert scale questions to assess current EHR tool use, when clinicians conduct documentation, and technology acceptance. An open-ended question asked clinicians to describe what EHR support for OW/OB care would look like if given a magic wand. We summarized responses using descriptive analyses and Chi Square tests for Likert Scale items and content analyses for open-ended answers to categorize common themes. Primary care clinicians use EHR tools but do not always believe they support workflow efficiency or enhance the quality of care delivered. Clinicians envisioned tools that can assist beyond information organization and knowledge support by automating routine documentation tasks. Future work will assess how engaging clinicians in tailoring design impacts acceptance and use of CDS tools.
Results: A total of 305 participants completed the survey (32.5% response rate); 74.4% identified as women, 57.4% attendings, 29.5% residents/fellows, 13.1% APPs, 40% reported ≥10 years in practice. Most clinicians document during the patient visit (90.5%), and many clinicians start documentation before a visit (56% of attendings, 63.3% of resident/fellows, 47.5% of APPs). While most clinicians reported using existing CDS tools in primary care (Table 1), less than half (45.7%) of attendings felt CDS tools increased clinical efficiency. Most (58.9%) residents/fellows believe CDS tools enhance the quality of care delivered, but only 40.6% of attendings and 47.5% of APPs agreed. In open-ended responses, clinicians offered suggestions for auto-populating information such as diagnosis codes, recommended lab orders, and patient education. However, some clinicians demonstrated reservations with EHR-based supports including feeling overwhelmed by the number of tools and systemic barriers to care, with the belief that EHR tools will not be able to address such barriers.
Conclusion(s):