Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 2
533 - Medical Team Practices Associated with Interpreter Alterations During Family-Centered Rounds
Publication Number: 533.117
- VP
Victoria Parente, MD (she/her/hers)
Assistant Professor
Duke University School of Medicine
Durham, North Carolina, United States
Presenting Author(s)
Background:
Robust evidence demonstrates inequities in communication during family-centered rounds for families with primary Language other than English (LOE). One contributor includes alterations during interpretation, which are common and can negatively affect family-centered communication. To evaluate medical team communication practices associated with interpreter alterations.
Objective:
Design/Methods:
We conducted an observational study of interpreter-supported family-centered rounds for Spanish-speaking families. All enrolled caregivers consented to audio record family-centered rounds. We transcribed audio-recordings verbatim and applied a priori defined codes to each interpreted segment of communication. We assessed measures of medical team communication including specific behaviors (e.g- use of jargon, total words/sentences), and interpreter alterations (omissions, additions, and substitutions) using previously described instruments. Two bilingual authors coded the encounters; transcripts were double-coded until reliability achieved. We used logistic regressions to evaluate the association between medical team communication measures as predictors for any interpreter alteration.
Results:
To date, six encounters have been coded for a total of 314 interpreted segments. Interpreter alterations of medical team and caregiver communication were common (Table 1); 210/314 (67%) interpreted segments had at least one alteration in interpretation. Substitutions were the most common alteration (119/314, 38%) followed by omissions (111/314, 35%) and additions (49/314, 16%). Omissions were strongly associated with the number of words and sentences used by the medical team (Figure 1). Interpreters were more likely to omit information when medical teams spoke 2 sentences (OR 2.0, 95% CI 1.0, 3.8), 3 sentences (OR 5.9, 95%CI 2.4, 14.6), and 4 sentences (OR 14.1, 95%CI 2.9, 68.7) compared to 1 sentence before pausing for interpretation. Substitutions were not associated with total words/sentences but were predicted by the use of medical jargon; the rate of at least one substitution was 62% vs 34% when medical jargon was used compared to not used (OR 3.2, 95%CI 1.6, 6.4). Interpreter alterations in communication during family-centered rounds are common. Medical team practices, such as infrequent pauses and use of medical jargon were significantly associated with interpreter alterations. To improve communication with LOE families, medical teams must abide by best practices for using an interpreter to facilitate more accurate interpretation.
Conclusion(s): 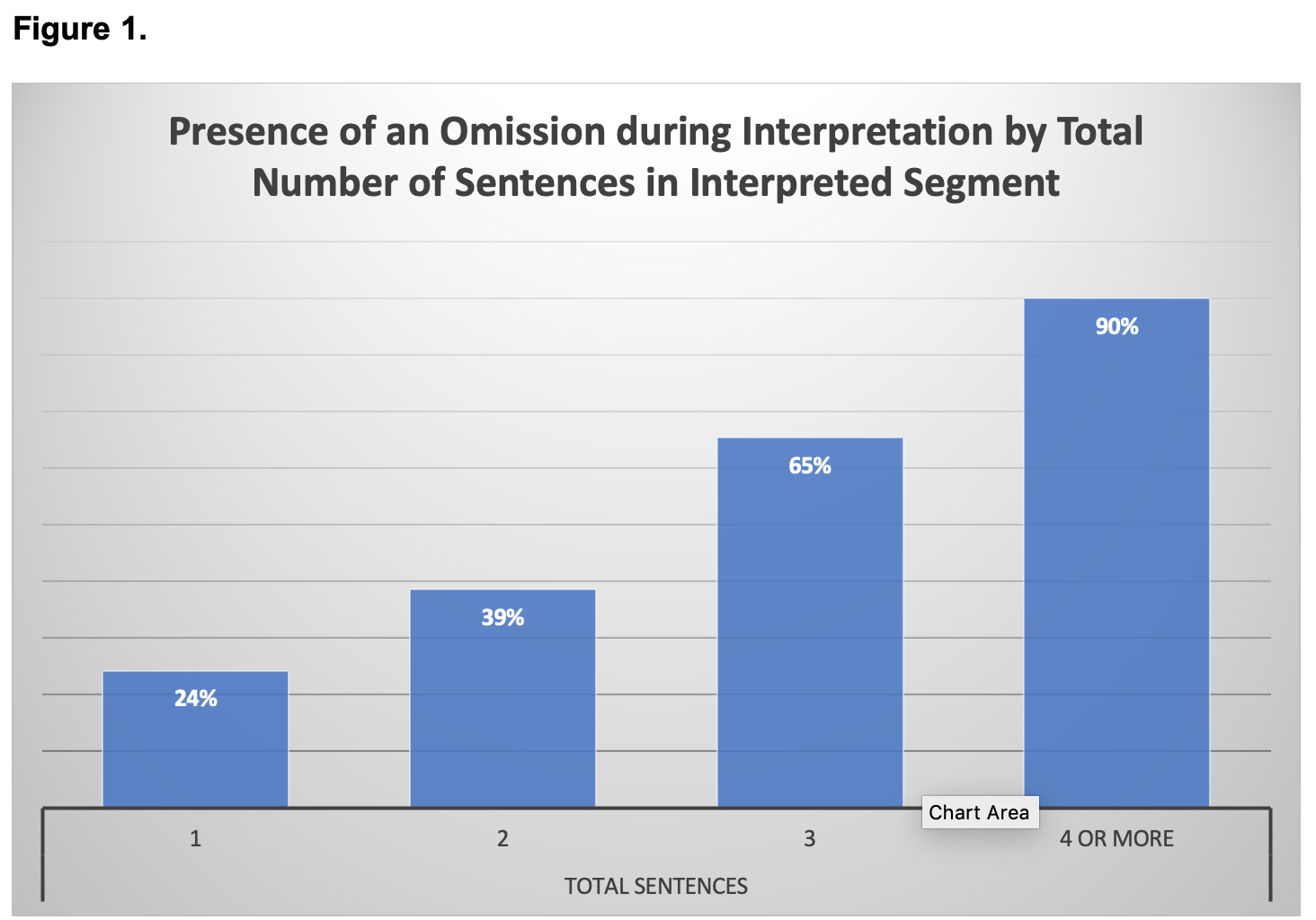
.png)
