Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 2
537 - The Language Equity Task Force: Addressing Language Equity for Hospitalized Patients and Families
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 537
Publication Number: 537.117
Publication Number: 537.117
Christina R. Rojas, Children’s National Hospital, Washington, DC, United States; Katherine W. Moore, Children's National Health System, Alexandria, VA, United States; Jaeho Chang, Children's National Health System, Washington, DC, United States; Enrique Escalante, Children's National Health System, Washington, DC, United States; Asha S. Payne, Children's National Health System, Washington, DC, United States; Christina Lindgren, Children’s National Hospital, Kensington, MD, United States; Joelle Simpson, Children's National Health System, Washington, DC, United States; Denice Cora-Bramble, Children's National Health System, Washington, DC, United States

Christina R. Rojas, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Children’s National Hospital
Washington, District of Columbia, United States
Presenting Author(s)
Background: Hospitalized children and families who prefer languages other than English (LOE) experience inequitable communication compared to their counterparts preferring English. These inequities are prevalent and extend across various hospitals, healthcare provider types, and specialties. While novel interventions targeting specific aspects of this inequity have been developed, the implementation of a holistic institutional strategy to promote language equity has not yet been described.
Objective: Develop a multidisciplinary task force focused on understanding and addressing inequities experienced by hospitalized patients and families preferring LOE.
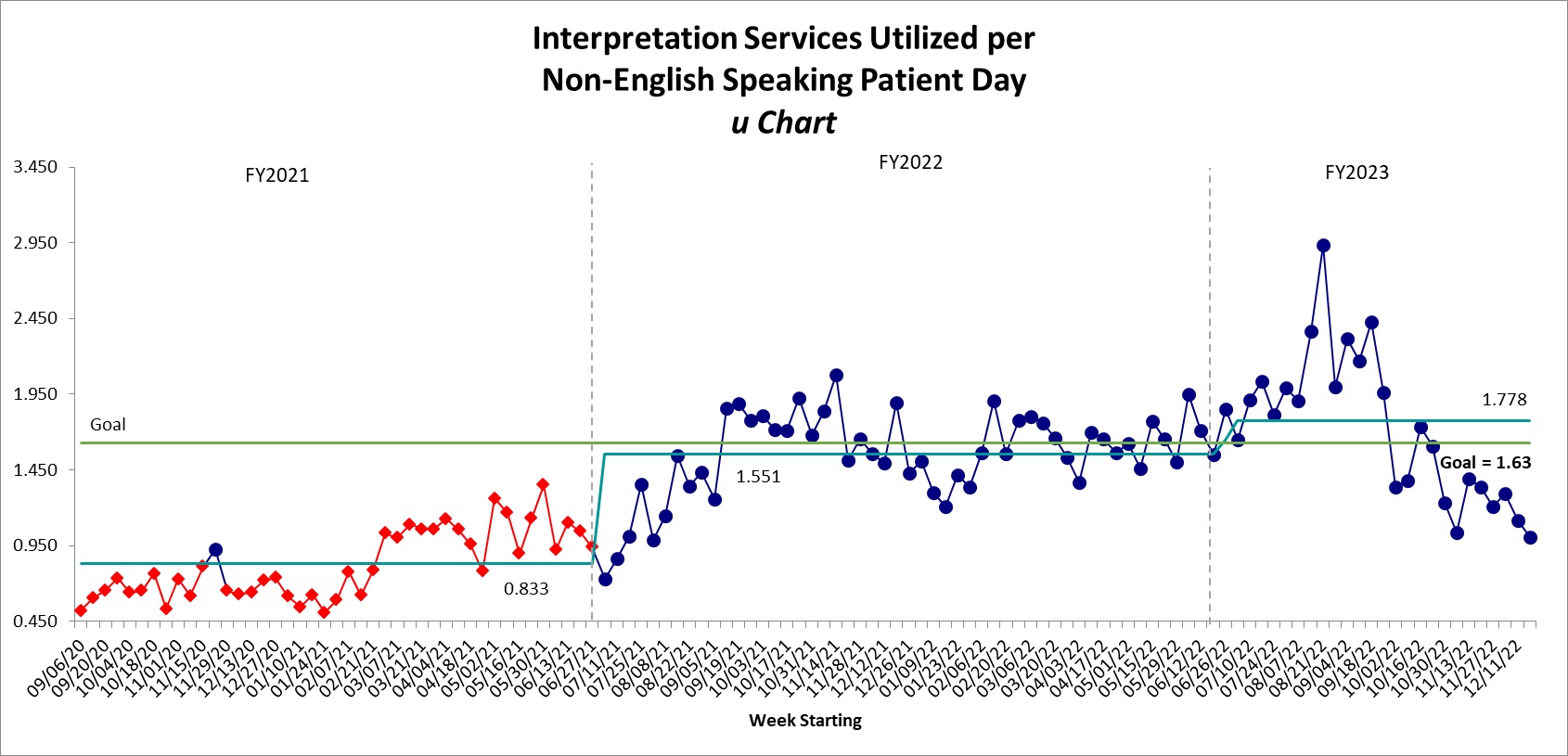
Design/Methods: A diverse group of stakeholders was assembled, including physicians from various specialties and levels of training, nurses, social workers, interpreters, and institutional leaders. Strengths-Weaknesses-Opportunities-Threats (SWOT) analyses and Gemba walks were conducted to determine institutional and task force priorities (Figure 1). Use of interpretation was identified as a core focus; statistical process control charts were developed to understand the scope of this inequity. Secondary priorities included language concordance of discharge instructions and accuracy of preferred language documentation in the electronic medical record.
Results: Data related to language equity was compiled into a comprehensive, user-friendly data dashboard, detailing patient and family preferred language, demographic information, and frequency of interpretation (Figure 2). Preliminary data analysis related to use of interpretation demonstrated that hospitalized patients and families preferring LOE experience less than 2 interpretation encounters per day of hospitalization (Figure 3); improvement efforts are ongoing. Additional task force efforts focused on promoting a culture that acknowledges and addresses inequities related to communication, including Grand Rounds and staff educational opportunities.
Conclusion(s): Significant inequities in communication for hospitalized children and families preferring LOE persist, particularly related to appropriate use of interpretation. Development of a multidisciplinary, institutionally sponsored task force can serve to focus and prioritize efforts to promote language equity.
.png)