Developmental and Behavioral Pediatrics: Autism
Developmental and Behavioral Pediatrics 2
562 - A Descriptive Analysis of Family Navigation Activities for Early Autism Diagnosis
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 562
Publication Number: 562.109
Publication Number: 562.109
Mattie G. Watts, Oregon Health & Science University School of Medicine, Portland, OR, United States; Mohadeseh Solgi, OHSU, Portland, OR, United States; Avneet Sidhu, Oregon Health & Science University School of Medicine, Portland, OR, United States; Michelle Tae, Help Me Grow, Beaverton, OR, United States; Joseline Raja-Vora, Providence Health Services, Portland, OR, United States; Eric Fombonne, Oregon Health & Science University, Portland, OR, United States; Abby Bush, Center for Outcomes Research and Education, Portland, OR, United States; Katharine E. Zuckerman, Doernbecher Children's Hospital at Oregon Health & Science University, Portland, OR, United States
.jpg)
Mattie G. Watts, BS (she/her/hers)
Medical Student
Oregon Health & Science University School of Medicine
Portland, Oregon, United States
Presenting Author(s)
Background: Autism Spectrum Disorder (ASD) can be identified as early as age two. However, many children experience delays in diagnosis. One reason for delayed diagnoses may be that caregivers of children with ASD have difficulty navigating health and education systems. Family navigators may help reduce delays in ASD diagnosis in under-resourced communities. This study relies on a secondary analysis of data collected in the Autism ALERT project, a randomized trial of telehealth-based family navigation for early ASD diagnosis and treatment, using family navigators.
Objective: Our objective was twofold: to estimate the number of navigator-to-family contacts needed to determine which navigation activities were most frequent, and to determine the efficacy of the navigation activities.
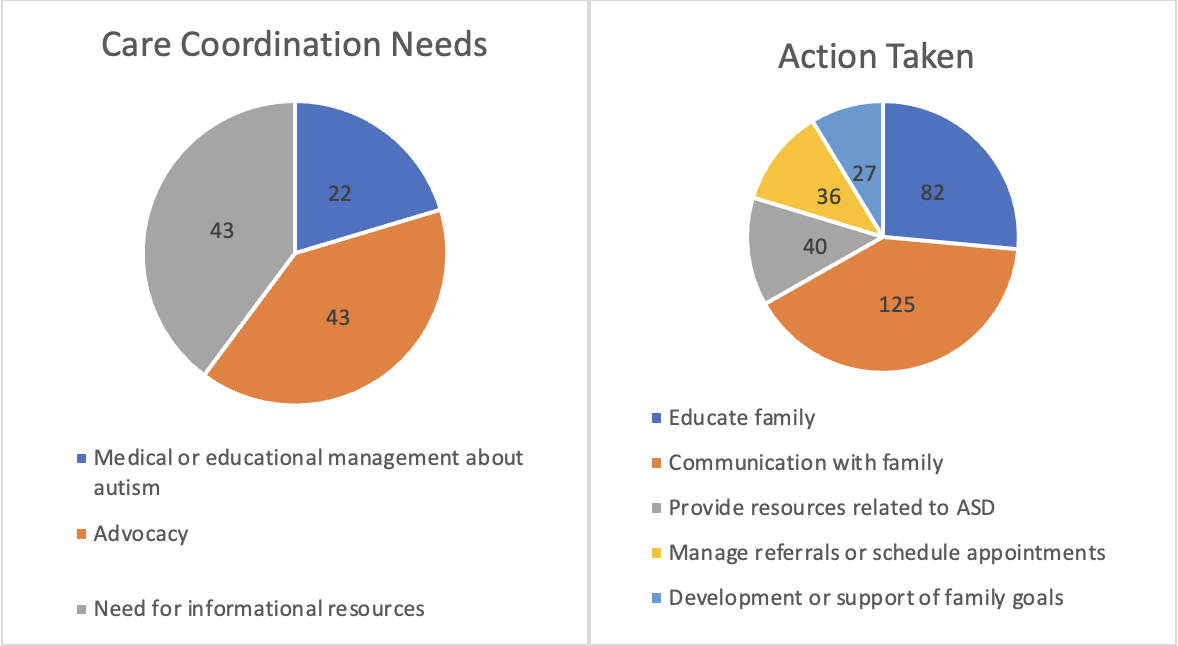
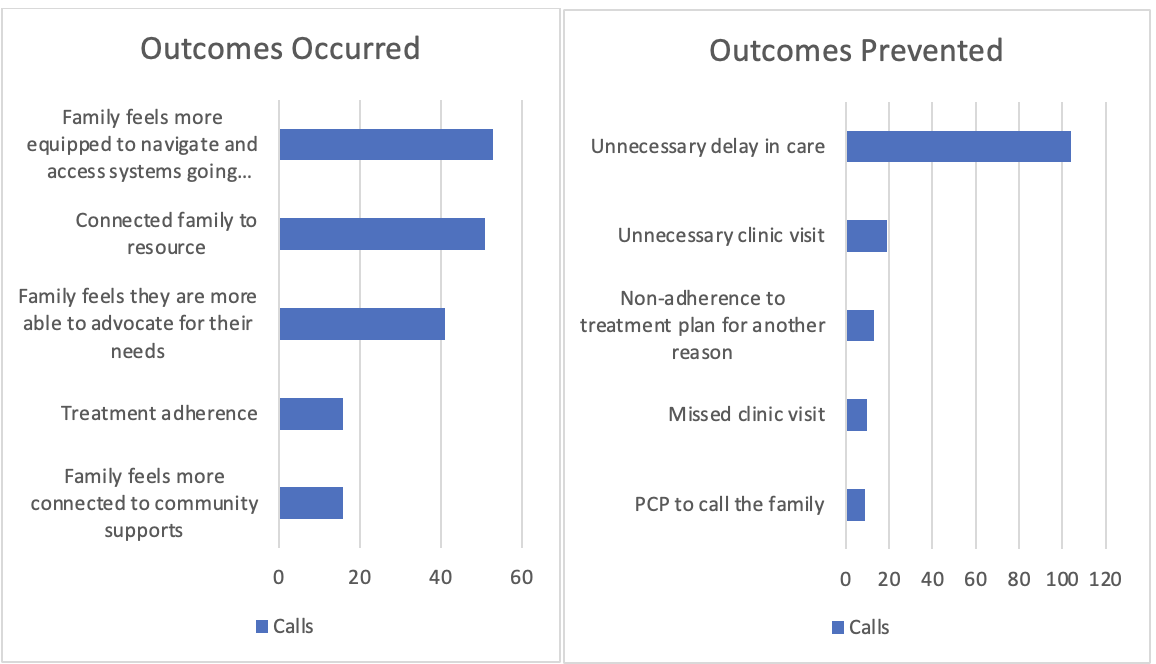
Design/Methods: We collected navigator-reported data from 32 families who received the Autism ALERT navigation intervention. Data was collected via the Care Coordination Measurement Tool (CCMT), a validated provider-completed measure. After each telehealth encounter with a family, the navigator filled out a CCMT survey. Survey data were used to assess: number of calls made by navigators, number of calls answered by families, median call time, care coordination needs met, actions taken, outcomes occurred, and outcomes prevented. Completed CCMT surveys were extracted from RedCap and analyzed with descriptive statistics.
Results: Of 352 phone calls made by navigators, 168 were answered by families. Median calls per family was 12 (Range 0-31); median call time was 7 minutes (Range 3-135 minutes). Most frequent navigator care coordination activities were medical/educational management of autism, family advocacy, and provided informational resources. Most frequent actions taken were educated family, communicated with family, provided ASD resources, managed referrals/scheduled appointments, and developed/supported family goals (Figure 1). Most frequent outcomes occurred were treatment adherence, connected family to resource, family equipped to navigate and access systems, family connected to community supports, and family able to advocate for their needs. Most frequent outcomes prevented were unnecessary clinic visit, missed clinic visit, PCP to call the family, and unnecessary delay in care (Figure 2).
Conclusion(s): Telehealth-based autism family navigation helps families access care, and was associated with improved process outcomes. Increased communication, family advocacy, and informational resources were frequently used strategies.