Hospital Medicine: Hospital Medicine Quality Improvement
Hospital Medicine 1
750 - QI Project to Improve Infant Safe Sleep Environment on the General Pediatric Wards
Publication Number: 750.119
Kristina M. Nazareth-Pidgeon, MD (she/her/hers)
Pediatric Hospitalist
Duke University School of Medicine
Raleigh, North Carolina, United States
Presenting Author(s)
Background: Following a successful QI project to improve adherence to the American Academy of Pediatrics (AAP) infant safe sleep guidelines [1] in our newborn nursery, our institution created a multidisciplinary “Safe Sleep Taskforce” and turned its attention to reducing the infants sleeping in unsafe environments while admitted to the General Pediatrics wards, as patients aged less than one year should also be following AAP guidelines.
Objective:
Our SMART goal was to improve the incidence of compliance with each of five components of a safe infant sleeping environment (appropriate location, position, bundling, crib flat and empty) to greater than 80% within 18 months.
Design/Methods:
An audit tool was created to record an infant’s sleeping environment during their admission to the General Pediatrics wards. A rapid-improvement QI approach was used, with PDSA cycles focusing on hospital policy, nursing education, and resident education.
Results:
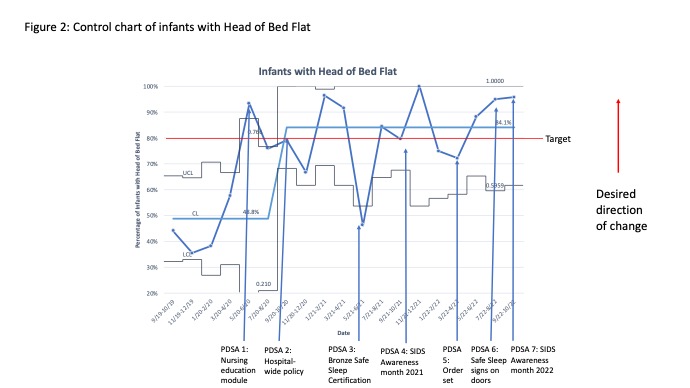
After collection of baseline data, it was found that two components of a safe sleep environment were already above the target of 80%. Infants were sleeping in an appropriate location 93.8% of the time, and there was no significant change in this during our project. Infants less than 4 months of age were sleeping appropriately on their back in 83.3% of time, and this increased to 97.8%. Infants that were bundled appropriately statistically significantly increased from 73.7% to 90.8% (Figure 1), and infant with the head of the bed flat statistically significantly increased from 48.8% to 84.1% (Figure 2), both meeting our SMART goal. Center line shift was noted in September of 2020 when the hospital-wide safe sleep policy went into effect. The number of infant sleep environments containing extra items decreased twice from 75.1% to 43.3% and then to 32.6% but this did not meet our target. All improvements were maintained until the end of the study period.
Conclusion(s):
A QI approach can be used on the General Pediatric wards to improve adherence to elements of the AAP’s infant safe sleep guidelines for patients under one year of age, but challenges still exist, particularly with removing extra items from the sleep space. Future directions include PDSA cycles to address these continued challenges and expanding audits to other hospital units.
.jpg)