Emergency Medicine: All Areas
Emergency Medicine 2
41 - The clinical impact of respiratory disease in children under the age of two during the 2021-2022 bronchiolitis season in the United Kingdom and Ireland
Publication Number: 41.111

Damian Roland, BMedSci, BMBS, FRCPCH, PhD (he/him/his)
Head of Service, Children's Emergency Department, Leicester Royal Infirmary
Leicester University and Hospitals
Leicester, England, United Kingdom
Presenting Author(s)
Background:
Interventions in 2020 to reduce the spread of SARS-CoV-2 led to a widespread reduction in childhood respiratory disease, including respiratory syncytial virus (RSV).
Objective:
Anticipating unusual disease dynamics, and the emergence of effective monoclonal antibody treatments, we planned a study to understand this out of season epidemic and use this dataset to gain an up-to-date understanding of the burden of disease in the 0-2 year age group.
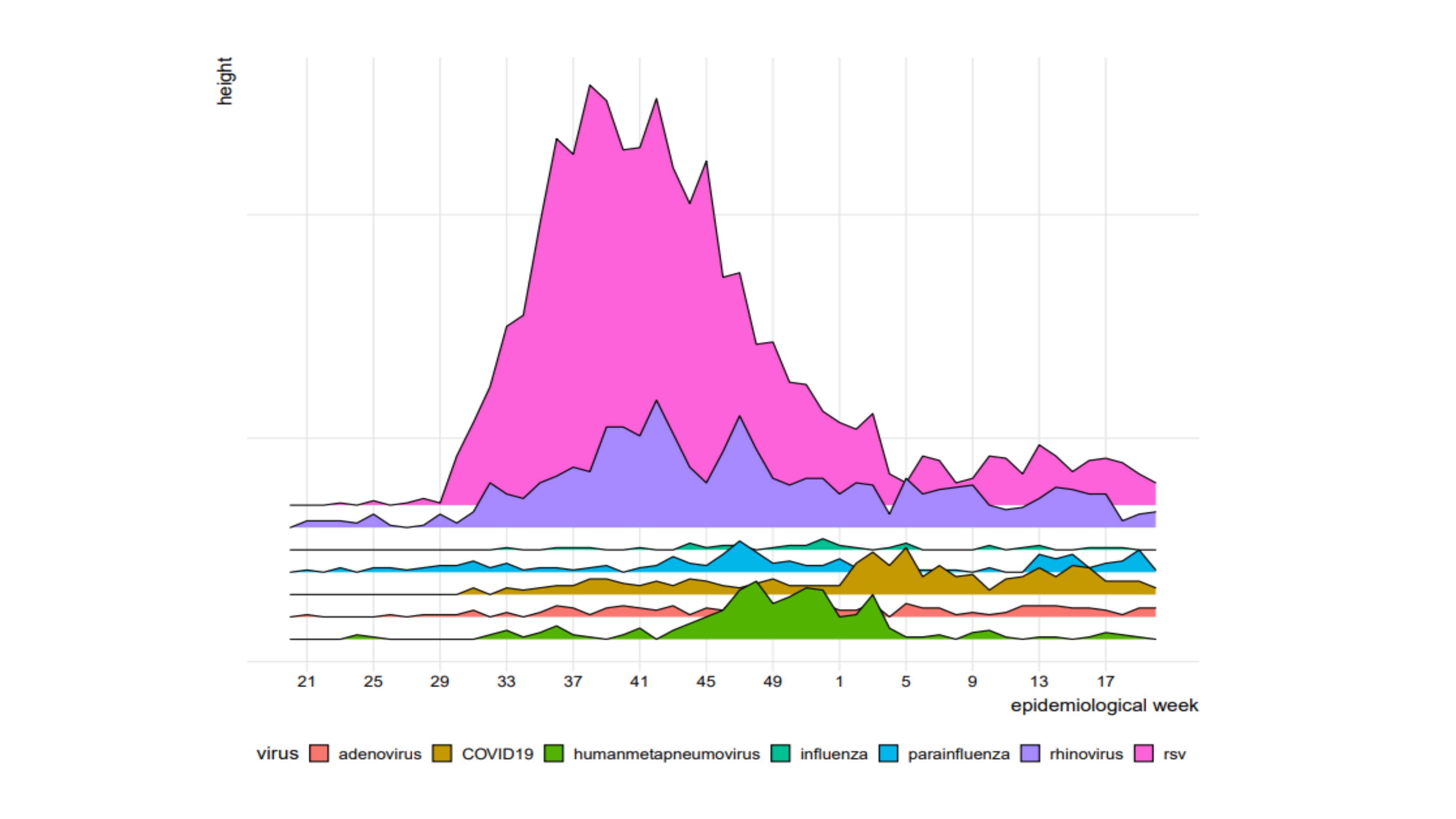
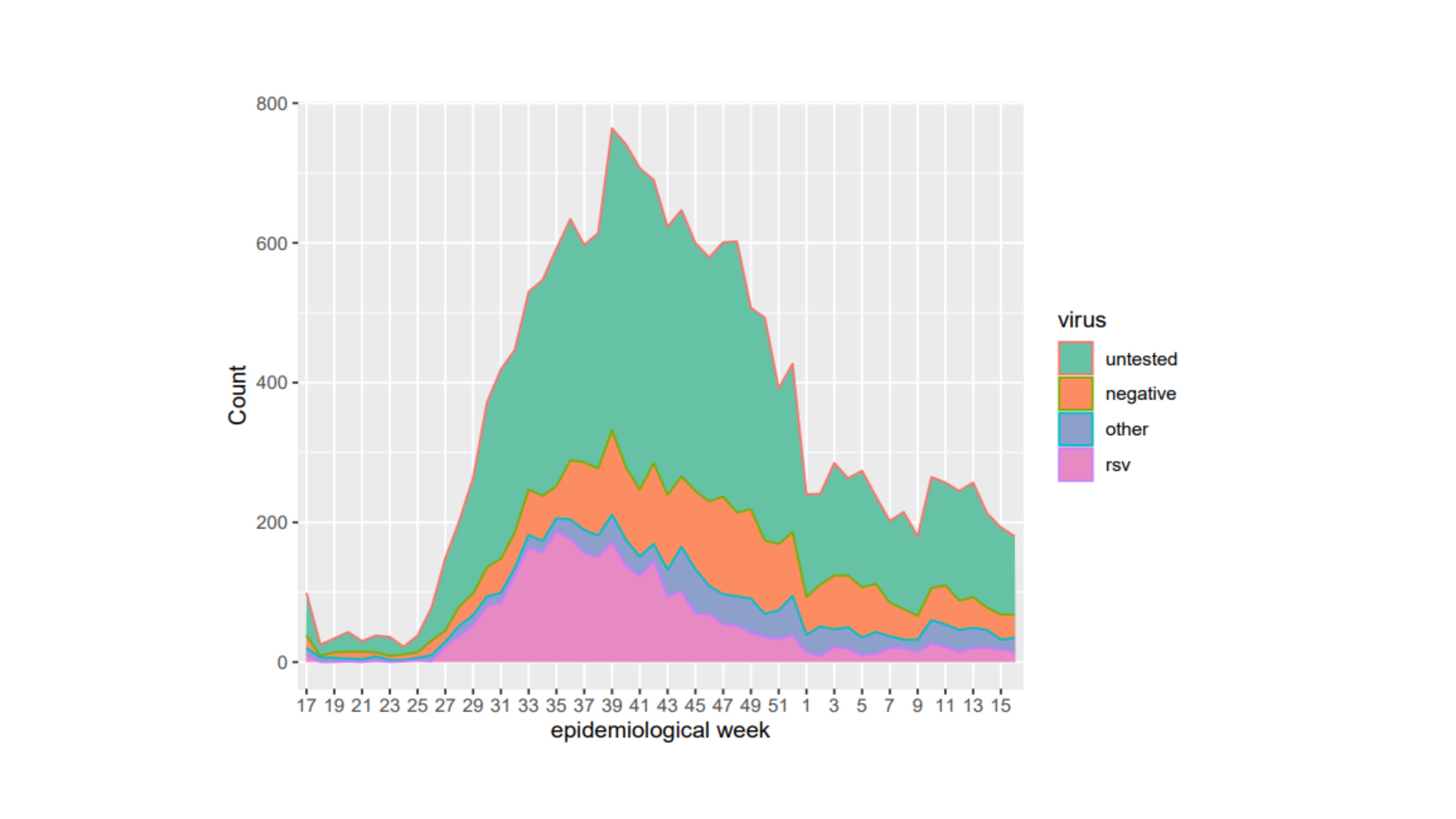
Design/Methods: We conducted a prospective observational cohort study (BronchStart) for children presenting with clinician-diagnosed bronchiolitis, lower respiratory tract infection or first episode of wheeze in 59 emergency departments across England, Scotland and the Republic of Ireland from 1 May 2021 onwards. We collected baseline data on patient demographics and clinical presentation, and follow-up data at 7 days. We used high-granularity clinical data from our study together with a national English admission dataset to infer the burden of disease in a typical year preceding the Covid-19 pandemic, and to provide an up-to-date estimate of the annual burden of disease to inform the implementation of anti-RSV interventions.
Results:
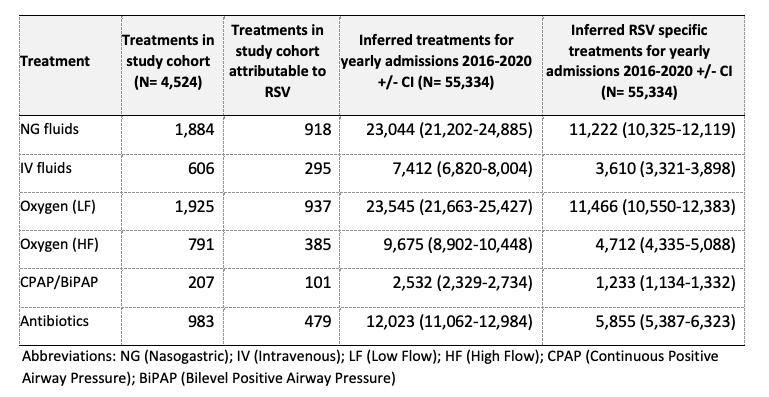
The BronchStart study collected data on 17,914 presentations for 17,179 individual children aged 0-2 years from the period 1 May 2021 to 30 April 2022. Of these 6,830 (38.1%) were admitted to hospital for further observation or treatment, 458 (2.6%) required care in a high dependency unit (HDU), and 155 (0.9%) were admitted to a paediatric intensive care unit (PICU). Of those admitted and tested for RSV, 41.8% were positive for the virus; 48.7% of those aged < 1 year of age tested positive for RSV. 84.5 % of those admitted to an observation unit, 78.1% of those admitted to a ward, 67.7% of those admitted to HDU and 50.3% of those admitted to PICU had no identified comorbidity. Using admissions data for England from the period 2016-2020, we estimate that every year 11,466 (95% CI 10,550-12,383) infants with RSV infection receive low flow oxygen, 4,712 (95% CI 4,335-5,088) high flow oxygen and 5,855 (95% CI 5,387-6,323) a course of antibiotic therapy. Our study provides an up-to-date estimate of the impact of acute respiratory disease in England in those aged 0-2 years. Although RSV was the major pathogen in this cohort, over 50% of admissions for respiratory disease in those aged < 1 year of age were not associated with the virus. The majority of these admissions, for all levels of care, were in previously healthy term born infants. This data aids assessment of the impact emerging interventions and planning health policy.
Conclusion(s):