Injury Prevention
Injury Prevention 1
133 - Changes in Pediatric Toxic Ingestions Due to the COVID-19 Pandemic
Publication Number: 133.121
.jpg)
Anoush Calikyan, BA, MA (she/her/hers)
Medical Student
Frank H. Netter MD School of Medicine at Quinnipiac University
New Haven, Connecticut, United States
Presenting Author(s)
Background:
Pediatric poisonings are a significant cause of morbidity and mortality. Studies have found that acute unintentional pediatric poisonings are often due to inadequate supervision and lack of familial and caregiver support, which has worsened during the COVID-19 pandemic due to the strains placed on family care and economic well-being.
Objective: This retrospective study evaluated the change in frequency of acute unintentional pediatric poisonings in Connecticut before and during the COVID-19 pandemic, as well as assessed any racial and ethnic disparities that existed within the years 2018-2021.
Design/Methods: A secondary analysis was conducted of emergency department (ED) discharge records from 2018-2021 involving children aged 0-17 years captured in the Connecticut Injury Surveillance System. International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes were used to identify ED discharges attributed to drug or substance overdose. Child age, sex, race/ethnicity, and insurance status were compared by pre-COVID (2018-2019) and COVID (2020-2021) periods. Rates were calculated per 10,000 ED discharges.
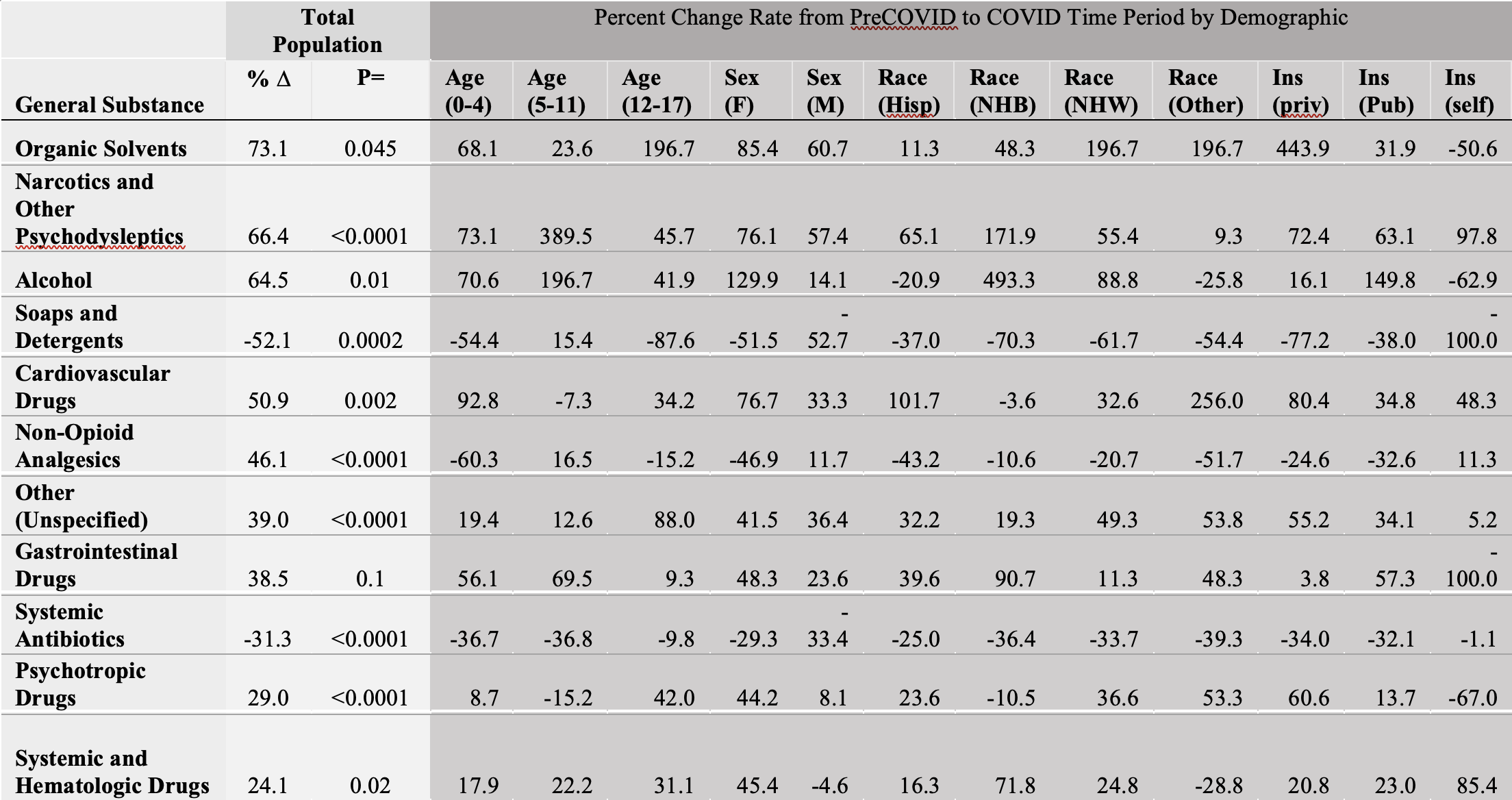
Results: We identified 867,162 total pediatric discharges during this time, of which 7,648 (< 1%) involved pediatric poisonings. Most pediatric poisonings involved substances labeled other/unknown and were then followed by non-opioid analgesics. The greatest change in poisonings which occurred after the start of the pandemic involved organic solvents, such as in degreasing and cleaning agents, which increased in emergency department visits by 73% (p=0.04) followed by narcotics and psychodysleptics at a 66% (P< 0.00001) increase and alcohol at 64% (p=0.01) increase. However, the changes in poisoning rates were not uniform across the population demographics; the greatest increases were observed in non-Hispanic black patients, who also had an increase in alcohol related emergency department visits by 493% (Table 1).
Conclusion(s): The results suggest that new strategies both to decrease pediatric poisonings as well as narrow the existing racial disparities are indicated. Improved policies that target accidental ingestions of young children as well as unintentional overdoses during teenage recreational drug use may be helpful. Furthermore, prevention efforts should target racial minorities, as our data has demonstrated an increased burden of poisoning on racial minority groups. Additional research is required to assess whether severity of poisoning and frequency of death due to poisoning have changed in addition to the increased frequency in poisoning.