Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 2
527 - Characterizing Healthcare Workers Ad-hoc Interpreter Usage and Barriers to Professional Interpreters for Hospitalized Limited English Proficiency Patients
Publication Number: 527.117
Raymond Parlar-Chun, MD
Associate Professor of Pediatrics
McGovern Medical School at the University of Texas Health Science Center at Houston
Houston, Texas, United States
Presenting Author(s)
Background:
The underuse of professional interpreters is an obstacle in attaining equitable healthcare for patients with Limited English Proficiency (LEP). Healthcare workers may experience barriers limiting the use of professional interpreters (PI).
Objective:
To characterize healthcare workers that utilize ad-hoc interpreters (AHI), describe barriers to professional interpreter services, and elicit reasons for usage of AHI.
Design/Methods:
A 27-question survey was disseminated to pediatric physicians, nurses, and respiratory therapists working at an urban tertiary care pediatric hospital. Questions included characteristics of respondents including role, frequency of interactions with LEP patients, speaking another language, and years worked at our hospital. Primary outcome was the self-reported percentage of LEP encounters using ad-hoc interpreters. Other questions included encountered barriers with interpreter services, and usage of AHIs. Open ended questions asking how interpreter services could be improved, and when AHIs were used allowed for qualitative analysis. Other analysis included descriptive statistics and t-tests for comparison testing.
Results:
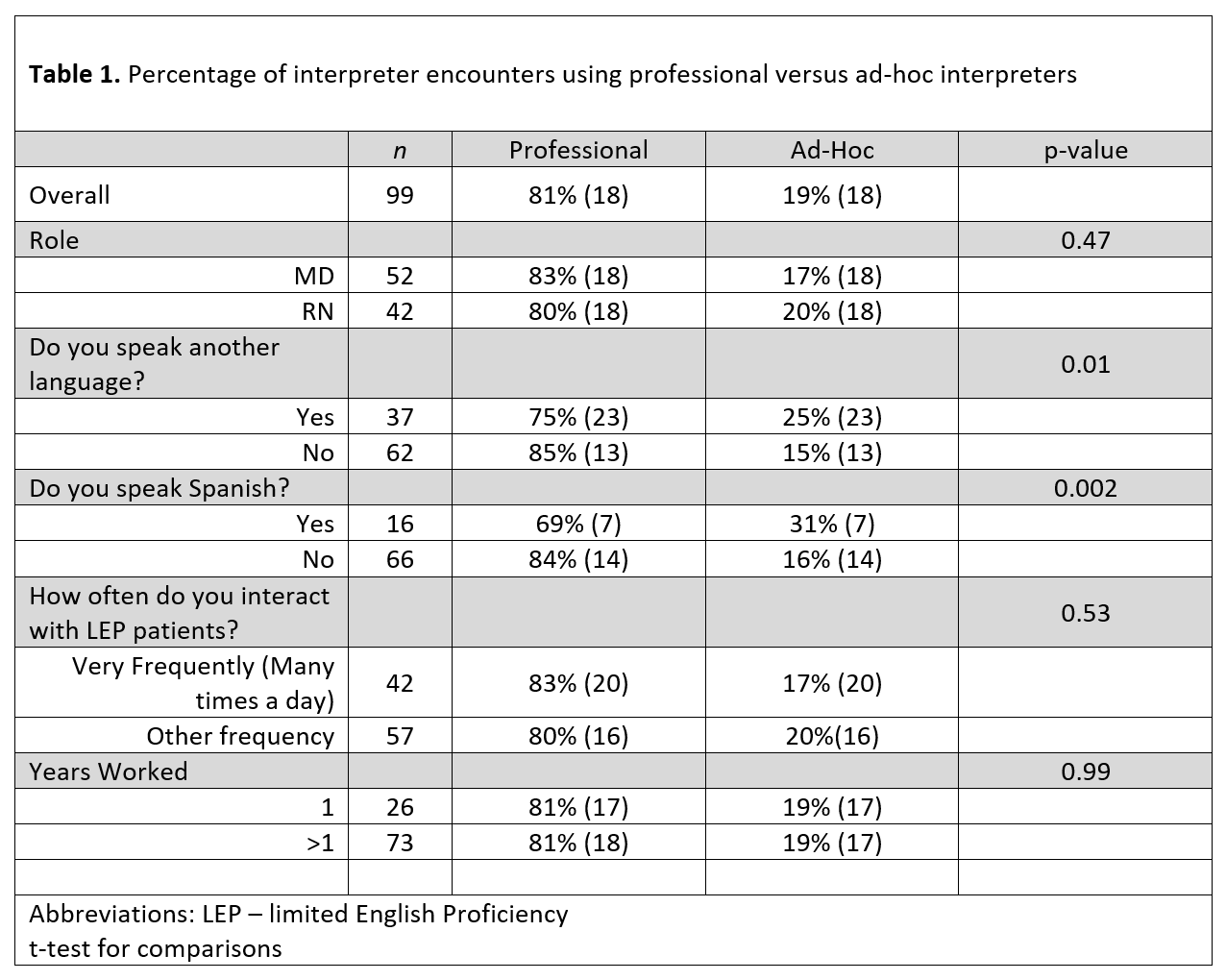
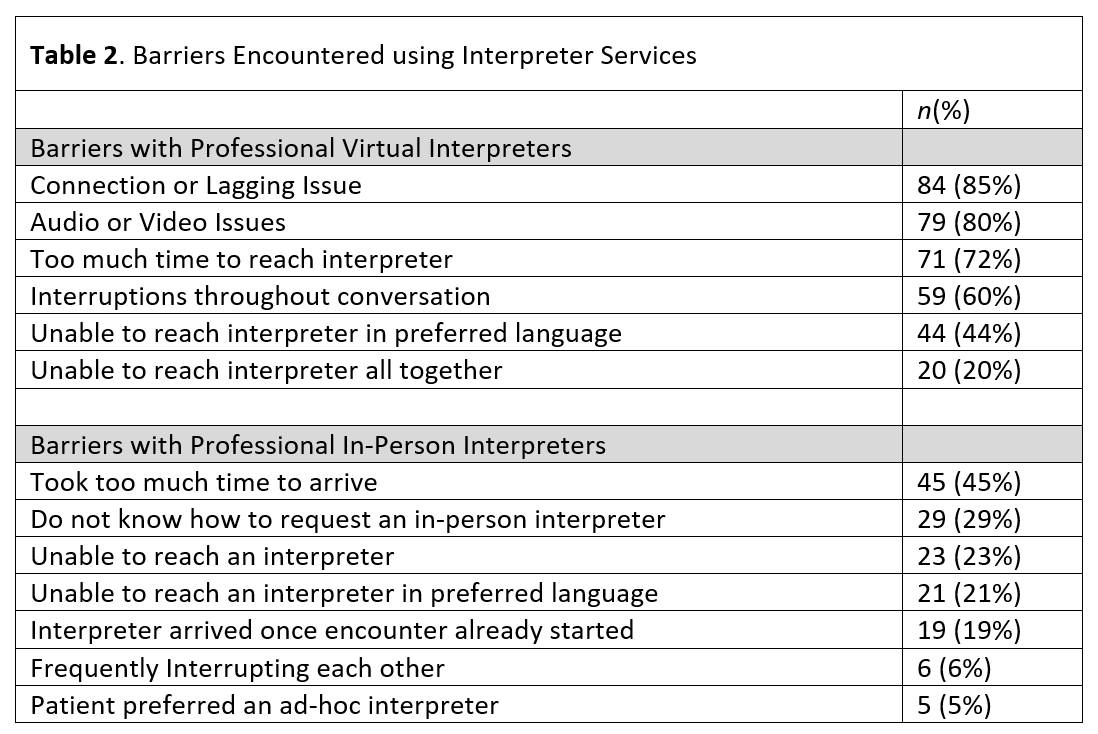
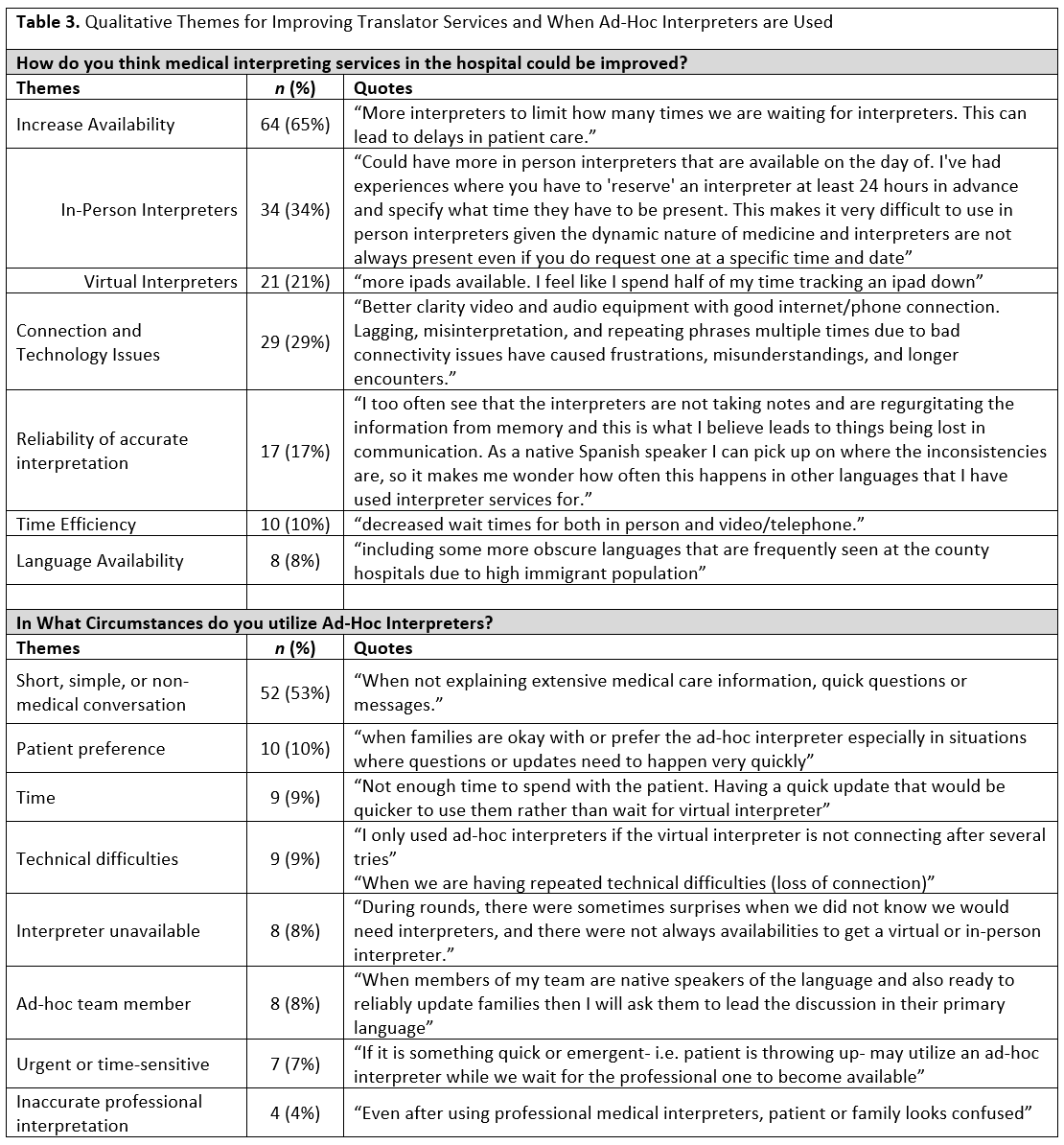
99 responses (52 MDs, 42 RNs, 5 RTs) were obtained with a response rate of ~41%. The majority of LEP encounters utilized professional interpreters (81%). There was no difference in usage of AHIs by role, years worked, or frequency of interaction with LEP patients. However, healthcare workers that spoke another language were more likely to utilize AHIs. TABLE 1. 83% of respondents had utilized AHIs, with the most common AHIs utilized being nurses (71%), residents (57%), and the other parent (52%). The most common reason not to utilize a PI was the presence of a bilingual co-worker (67%). The most common theme for AHI use were for short or non-medical conversation (53%). The most common barrier encountered for virtual interpreters were connection issues (85%), and the most common barrier for in-person interpreters were taking too long to arrive (45%) TABLE 2. Increasing interpreter availability was the most common theme to improve interpreter services overall (65%). TABLE 3.
Conclusion(s):
We find 1 in 5 encounters with LEP patients are done without professional interpreting services. Healthcare workers that spoke another language were more likely to utilize AHIs, perhaps reflecting enough familiarity with the language to perceive not needing a professional interpreter. We describe common barriers to services, and future studies should focus on interventions aimed to reduce these barriers while increasing the availability of professional interpreters.