Mental Health
Mental Health 3
720 - Trends in Pediatric Mental Health Visits to Three Tertiary Care Northern California Emergency Departments during the First Year of the COVID-19 Pandemic
Publication Number: 720.328

Victoria T. Chi, MD (she/her/hers)
Resident
Lucile Packard Children's Hospital Stanford
Mountain View, California, United States
Presenting Author(s)
Background:
The COVID-19 pandemic has exacerbated the growing mental health crisis among children. Changes in emergency department (ED) visit patterns may be a result of pandemic-driven mental health emergencies.
Objective:
To evaluate patient and community-level factors associated with mental health visits to three pediatric EDs in the San Francisco (SF) Bay Area during the first year of the COVID-19 pandemic compared to pre-pandemic years.
Design/Methods:
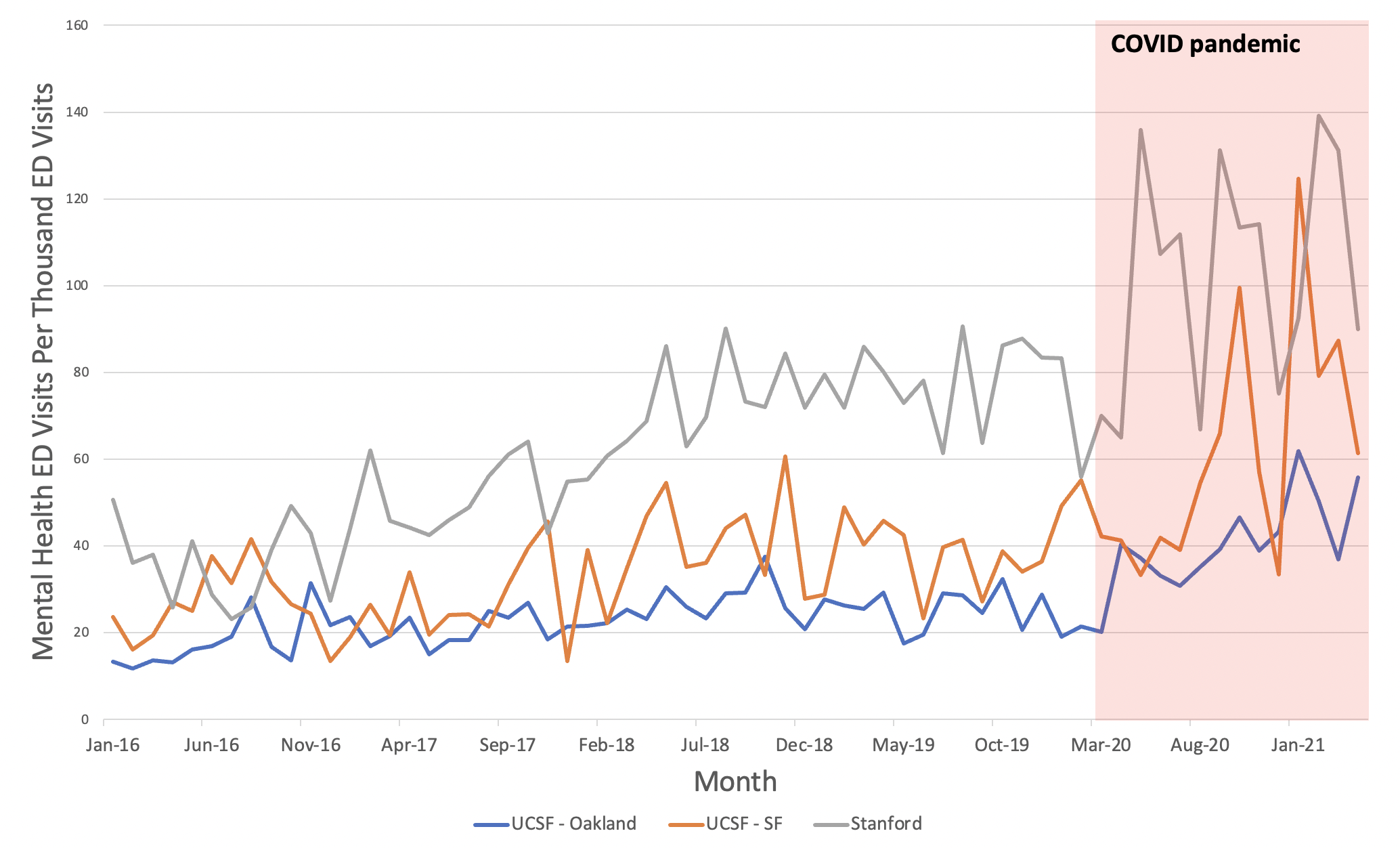
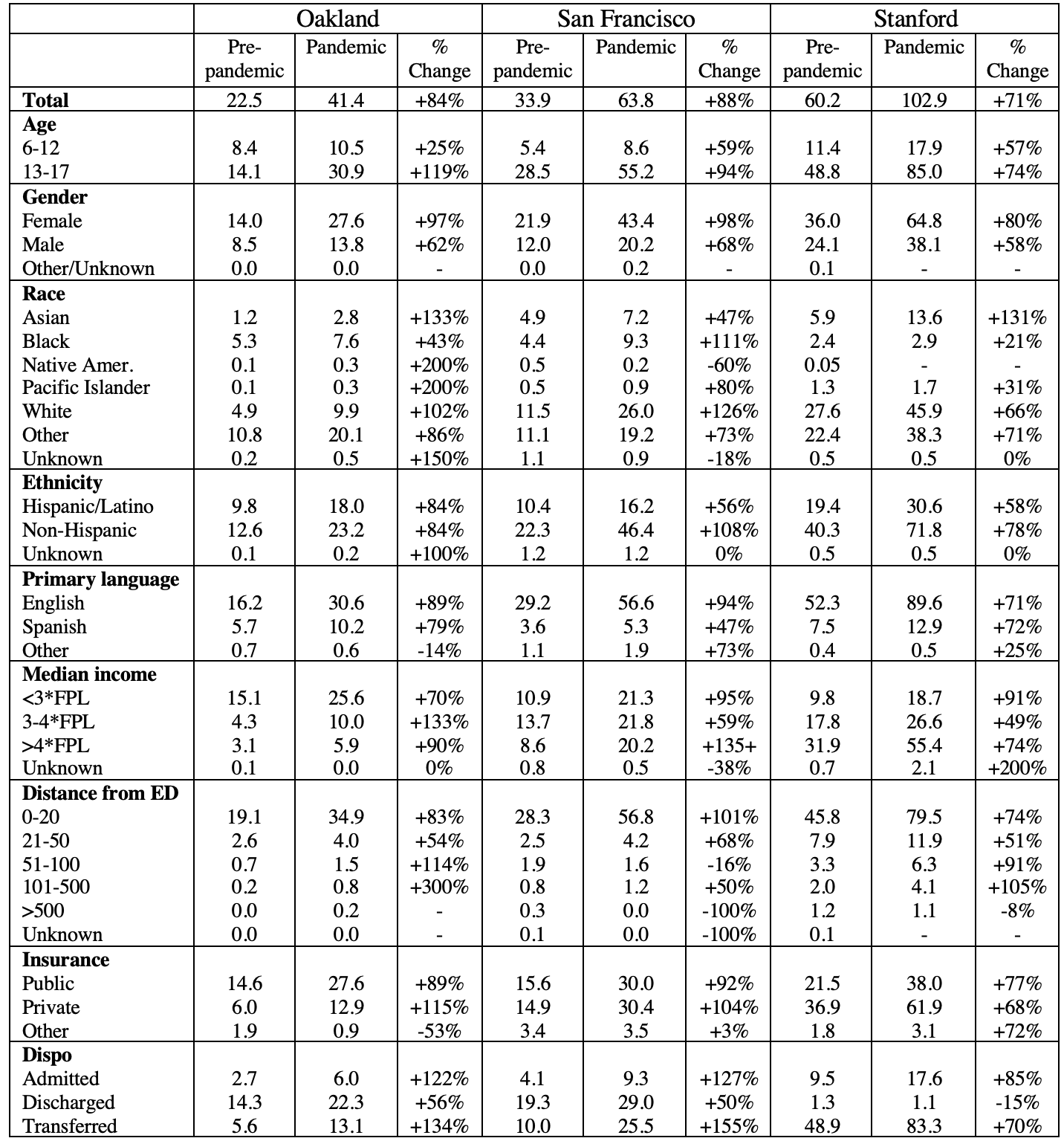
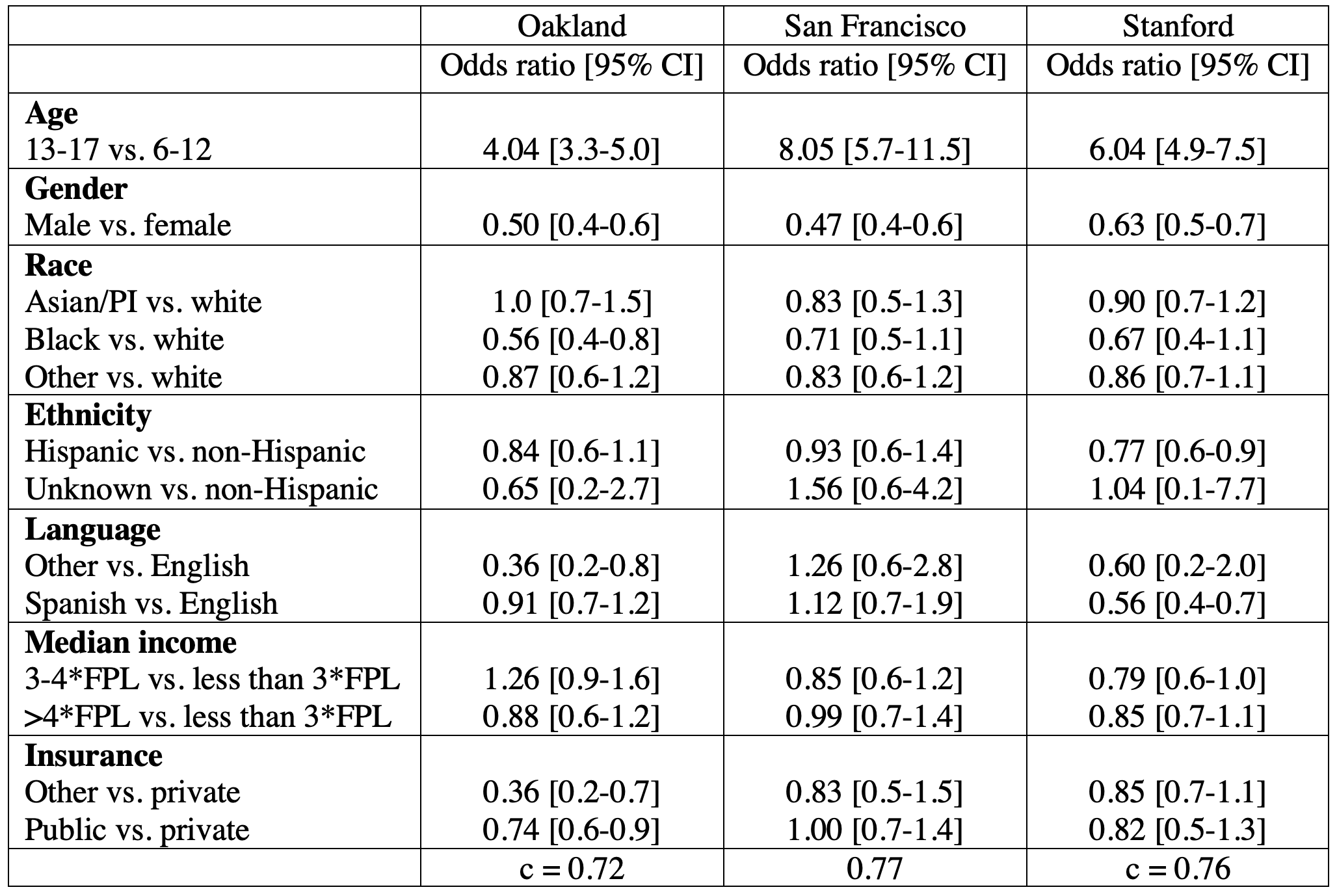
We extracted electronic health record data of children aged 6-17 years from three pediatric EDs. We compared the number and rates of mental health and total all-cause ED visits at each site during the first year of the pandemic (3/17/2020-4/30/2021) to the prior four years of data (1/1/2016-3/16/2020). We defined mental health ED visits as visits with a primary diagnosis of a new or pre-existing mental health disorder, classified by ICD-10 code and sorted using Clinical Classifications Software (CSS). Mental health was defined as a psychiatric (mood, anxiety, psychotic, or eating) disorder, suicidal ideation/attempt, or substance use. We examined age, sex, race/ethnicity, insurance type, and median household income based on residential zip code. We conducted multivariable regression analysis with the primary outcome variable of ED mental health diagnosis. Total all-cause pediatric ED visits declined by 45% (from 2,997 to 1,651 per month) during the first year of the pandemic compared to the 4-year pre-pandemic period. However, mental health ED visits increased by 3% (from 102 to 105 visits per month). The first pandemic year was associated with higher odds of ED diagnosis with mood disorders, anxiety disorders, and suicidal ideation/attempts compared to the pre-pandemic period. Adolescents had increased odds of all mental health diagnoses. At some sites, Black children, children who speak a primary language other than English, and children with public insurance (Medi-Cal) had lower odds of ED mental health diagnoses during the pandemic, controlling for other demographic factors. All EDs had similar results, despite serving different patient populations and volumes.
Results:
Conclusion(s):
Our study demonstrates an increase in mental health ED visits during the first year of the pandemic, compared to the pre-pandemic period, across the SF Bay Area. Changes in the demographic distribution of ED mental health visits may be caused by increased prevalence of mental health conditions or decreased access to outpatient mental health care. Overall, care systems must be strengthened to address the ongoing mental health crisis and particularly to protect adolescents.