Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 3
551 - Racial, Ethnic, and Economic Disparities in Ambulatory Pediatrics Patient Family Experience Metrics
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 551
Publication Number: 551.118
Publication Number: 551.118
Margaret N. Jones, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Michael Ponti-Zins, Cincinnati Children's, Cincinnati, OH, United States; Melinda C. MacDougall, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Shelley Ehrlich, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Ndidi Unaka, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Samuel P. Hanke, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Mary Burkhardt, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Alexandra Corley, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Kristen A. Copeland, Cincinnati Children's, Cincinnati, OH, United States; Andrew F. Beck, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States

Margaret N. Jones, MD FAAP (she/her/hers)
Academic General Pediatrics Fellow
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Patient family experience (PFE) metrics are used by pediatric healthcare institutions to measure perceived healthcare quality. PFE metrics are linked to patient outcomes. To our knowledge, no studies have used PFE data as a tool for measuring how families experience racism in pediatric settings or to inform interventions aimed at mitigating the effects of that racism on measurable outcomes.
Objective: To quantify racial, ethnic, and economic disparities in ambulatory pediatric PFE metrics.
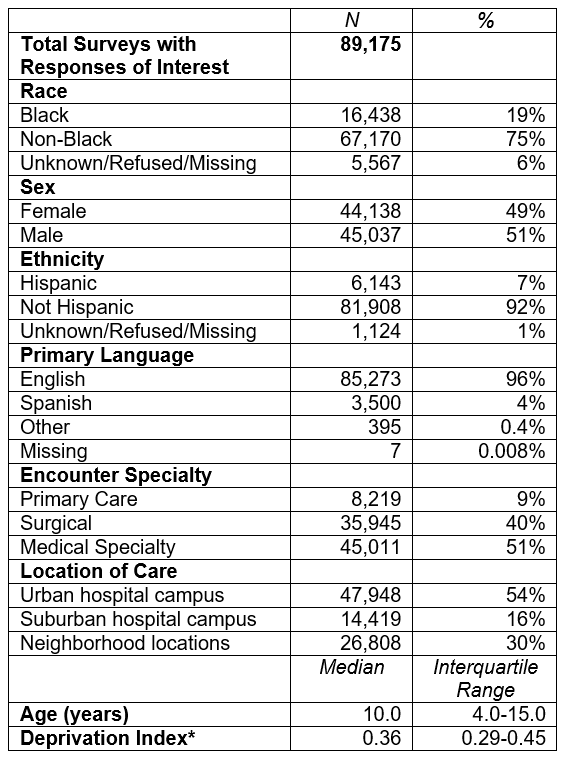
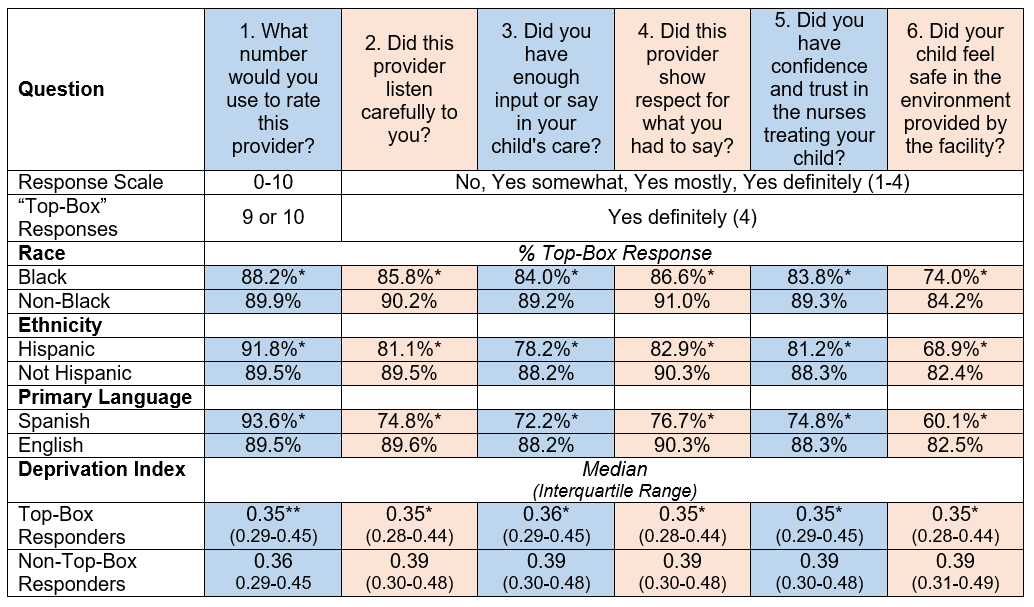
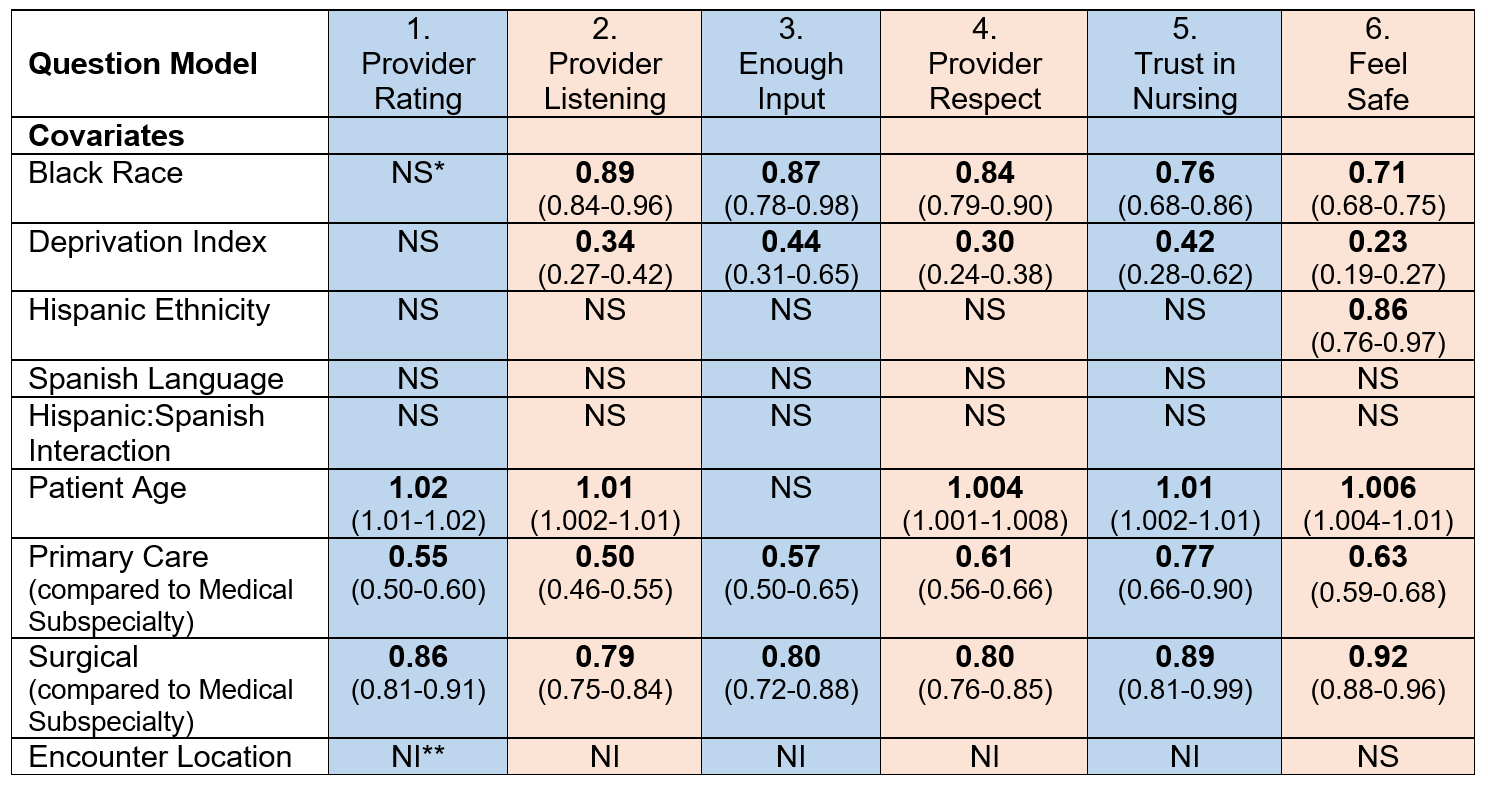
Design/Methods: We performed a retrospective review of PFE survey responses from all ambulatory medical encounters at a large, urban children’s hospital June 1, 2020—May 31, 2022. PFE surveys are administered by National Research Corporation within a week after clinical encounters. Outcomes included PFE survey scores for questions focused on overall experience, respect, and safety. We categorized outcomes using the industry standard metric of “top-box” score as a 9 or 10 for questions on a 10-point scale or as 4 on a 4-point scale. The primary covariate of interest was patient race, categorized as Black or non-Black. Secondary covariates included patient ethnicity, primary language, and neighborhood-level socioeconomic deprivation (quantified using a census tract-level Deprivation Index (DI) linked to geocoded patient addresses). We additionally controlled for patient sex and age, and encounter specialty and location of care. We evaluated differences in PFE survey scores by race and secondary covariates using bivariate analyses and multivariable logistic regression.
Results: A total of 89,175 PFE surveys were included in our analysis (Table 1). In bivariate analyses, Black patients had lower odds of choosing top-box responses to all questions of interest (Table 2). For example, 74.0% of Black patient caregivers responded, “Yes definitely” to the question, “Did your child feel safe in the environment provided by the facility?” compared to 84.2% of non-Black patient caregivers (p< 0.0001). Similar disparities were present for patients of Hispanic ethnicity, those who spoke Spanish, and those from tracts with greater DI. In multivariable analyses (Table 3), Black patients and patients from tracts with greater DI had significantly lower odds of top-box responses for 5 of 6 assessed questions.
Conclusion(s): We found previously unreported racial, ethnic, and economic disparities in ambulatory pediatric PFE outcomes. PFE metrics may be a useful tool for measuring how families experience racism and other forms of oppression. These metrics can guide parent-informed interventions aimed at equitably improving experience.