Emergency Medicine: All Areas
Emergency Medicine 2
36 - Impact of High Flow Nasal Cannula Flow Rates on Clinical Outcomes in Children with Bronchiolitis
Publication Number: 36.111
- NK
Nirupama Kannikeswaran, MBBS (she/her/hers)
professor of pediatrics and emergency medicine
Childrens Hospital ofMichigan
Detroit, Michigan, United States
Presenting Author(s)
Background:
Despite widespread use of high flow nasal cannula (HFNC) in treating children with bronchiolitis, considerable variation exists in flow rates used, and the effect of initial flow rate on clinical outcomes is poorly understood.
Objective: The objective was to evaluate the impact of initial HFNC flow rates on escalation of care (need for positive pressure ventilation (PPV)) and intensive care unit (ICU) transfer in children with bronchiolitis.
Design/Methods: We conducted a secondary analysis of retrospective study of children < 2 years of age requiring HFNC for bronchiolitis in a free standing children’s hospital. Children requiring immediate PPV or ICU admission at presentation, and those with underlying medical condition were excluded. The study timeframe, 10/1/2018 to 4/30/2022, included implementation of a revised institutional bronchiolitis clinical pathway in 2021 which recommended weight-based initiation of HFNC at 1.5 liters/kg up to a maximum of 2 liters/kg or 20 liters and a standardized weaning protocol. Previously, HFNC initiation was age-based, with starting rates of 8L for children 6-24 months. We evaluated the effects of three HFNC flow rates < 1.0 L/kg/ min (low), 1- 1.5 L/kg/min (medium), and >1.5 L/kg/min (high) on need for PPV, ICU transfer, time on HFNC, and hospital length of stay (LOS).
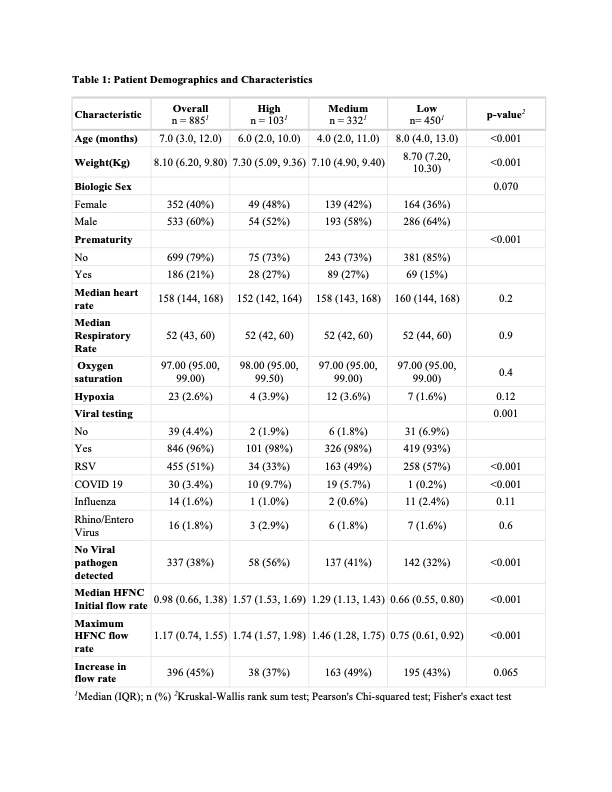
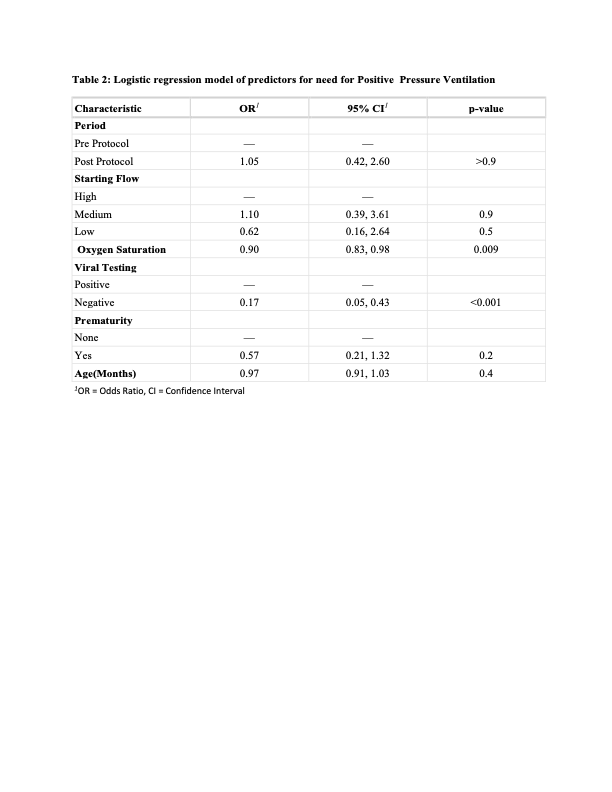
Results: Data on 885 children were analyzed with breakdown in the initial flow rates as follows: low (n=450, 50.8%), medium (n=332, 37.5%) and high (n=103, 11.7%). There were significant differences in age, weight, history of prematurity, viral testing, initial and maximum high flow rates between the three groups. However, there was no difference in the proportion of patients who required an increase in flow rate from initial between 3 groups (table 1). There were no significant differences in the need for PPV (High: 7.8% vs. medium: 9.3% vs. low: 8.2%, p=0.8) or ICU transfer (High: 4.9% vs. medium: 6.0% vs. low: 3.8%, p=0.3). However, children in the low flow rate group had a significantly longer median time on HFNC [High: 29 (18,45) vs. medium: 29 (16,50) vs. low: 39 (25,63), p< 0.001] as well hospital LOS [High: 41 (27,59) vs. medium: 42 (29,66) vs. low: 50 (39, 75), p< 0.001]. Logistic regression showed that other than negative viral testing, none of the factors, including initial HFNC flow rate, were associated with the need for PPV(table 2).
Conclusion(s): Initial HFNC flow rates did not impact need for escalated care in children with bronchiolitis. However, low flow rates were associated with longer HFNC treatment time and hospital LOS likely due to lack of standardized weaning protocol.