Hospital Medicine: Newborn Care
Hospital Medicine 2
756 - Car seat tolerance screening implementation and outcomes: Findings from a multi-site study through the Academic Pediatric Association's BORN Network
Publication Number: 756.12

Skye McLaurin-Jiang, MD, MPH (she/her/hers)
Assistant Professor of Pediatrics
Texas Tech University Health Sciences Center School of Medicine
Amarillo, Texas, United States
Presenting Author(s)
Background:
Previous studies identified variation in car seat tolerance screening (CSTS) performance among preterm infants in the United States. How variation in implementation impacts CSTS outcomes in newborns is unknown.
Objective: To explore whether infant-level factors were associated with CSTS practices and outcomes in a multi-site study via the Academic Pediatric Association’s Better Outcomes for Research through Newborns (BORN) Network.
Design/Methods: Electronic health record (EHR) data was extracted on infants discharged from level 1 (well-baby) newborn nurseries (NBNs) over a 6-year period (Jan 2015- Dec 2020) in 12 sites across the US. A cross-sectional survey obtained the CSTS criteria and NBN characteristics of each site. BORN sites that used EPIC EHR and had CSTS guidelines during the study period were eligible. Infants discharged from the neonatal intensive care unit, < 35 weeks, or < 1.8kg at birth were excluded. Chi-square tests examined the association of infant characteristics with receipt of CSTS and CSTS outcomes. Multivariable logistic regression models examined whether CSTS outcomes varied based on infant-level characteristics after adjusting for possible confounders.
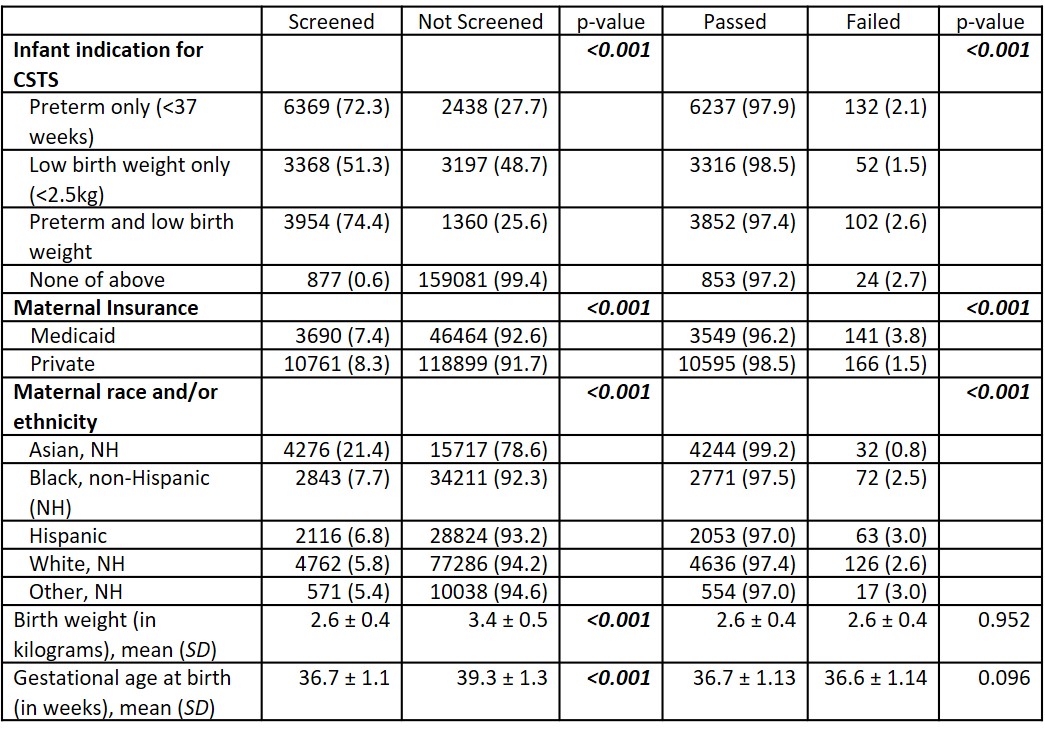
Results: Twelve hospitals contributed data on 180,644 infants. Hospital characteristics and guidelines for CSTS implementation are described in Table 1. Adherence to each site’s own CSTS criteria ranged from 16 - 100% and CSTS failure rates ranged from 0.7 – 9.9% across the 12 hospitals. Infant characteristics associated with undergoing CSTS and CSTS outcomes across the entire cohort are summarized in Table 2. Preterm, low birthweight infants were more likely to fail the CSTS than preterm only or low-birth-weight only infants (respectively, 2.6% vs 2.1% vs 1.5%, p< 0.01). Maternal insurance and race/ethnicity were associated both with receiving a CSTS and CSTS outcomes (Tables 2 and 3). Maternal insurance of Medicaid was associated with 2.3 times greater adjusted odds of CSTS failure (95% CI: 1.8, 3.0) while Asian, non-Hispanic race/ethnicity was associated with 0.74 times lower adjusted odds of failing the CSTS (95% CI: 0.2, 0.4), Table 3.
Conclusion(s): There is variation at multiple levels of CSTS implementation: (1) infant characteristics prompting screening, (2) definition of failure, (3) each hospital’s adherence to its own criteria, (4) failure rates. In addition, CSTS may be less consistent and CSTS outcomes may be poorer for infants with public compared to private insurance. Addressing variation at multiple levels of CSTS implementation has potential to improve equitability of practice.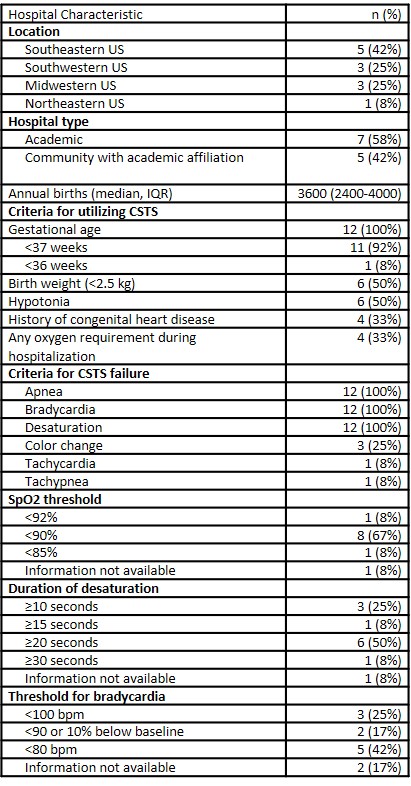
.jpg)
