Mental Health
Mental Health 1
578 - Effects of Virtual Learning on Children's Mental Health
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 578
Publication Number: 578.126
Publication Number: 578.126
ELIZABETH HISLE-GORMAN, Uniformed Services University, Bethesda, MD, United States; Madeline Dorr, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Gaithersburg, MD, United States; Apryl Susi, Henry M. Jackson Foundation at USUHS, GWU, Bethesda, MD, United States; Elizabeth H. Lee, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Annandale, VA, United States; Binny Chokshi, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Washington, DC, United States; Cade M. Nylund, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States

Elizabeth Hisle-Gorman, MSW, PhD (she/her/hers)
Associate Professor
Uniformed Services University
Bethesda, Maryland, United States
Presenting Author(s)
Background: Public health measures necessary to contain the spread of COVID-19 shifted education to a virtual interface. Virtual learning (VL) differed markedly by state ranging from 0-94% of the 2020-21 school year. While multiple studies have indicated adverse pandemic related effects on child and adolescent mental health, the impact of VL is largely unknown.
Objective: To explore the relationship between percentage of time in VL and the mental healthcare needs of children and youth during and following VL.
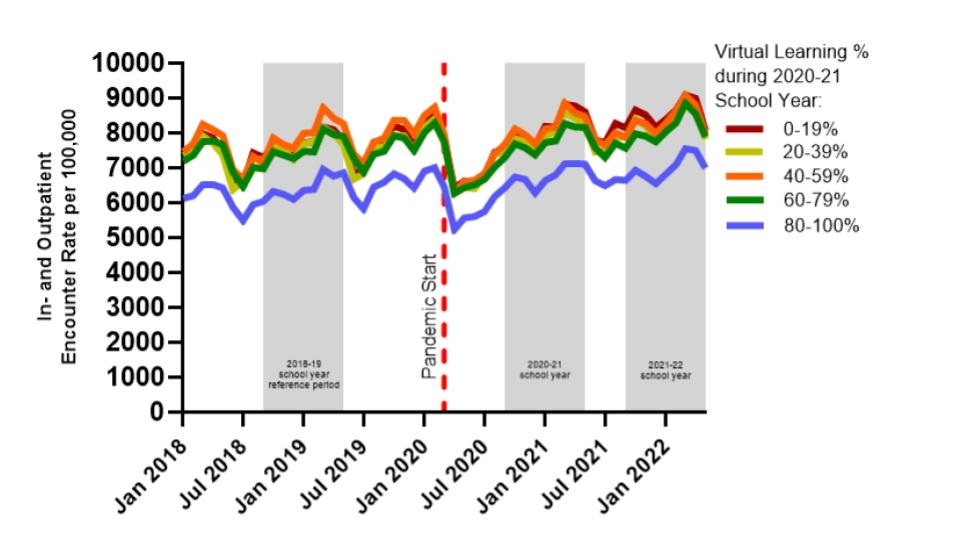
Design/Methods: A retrospective monthly cross-sectional study using military health system data explored mental healthcare use for children aged 5-18 in the 2020-21 (widespread virtual instruction) and 2021-22 (return to in-person) school years as compared to 2018-2019 (last full pre-pandemic school year). States were grouped by % VL (0-19, 20-39, 40-59, 60-79 and 80-100%) using Burbio school tracking data, and children were categorized by 2020-21 state of residence. In- and outpatient mental healthcare visits were identified by ICD-10 code. Pre-pandemic (2018-19) care rates different by state VL level, which necessitated stratified analysis (Figure 1). Wilcoxon Rank sum test compared group demographics. Poisson regression analyses determined rates of in- and outpatient mental healthcare visits by school year.
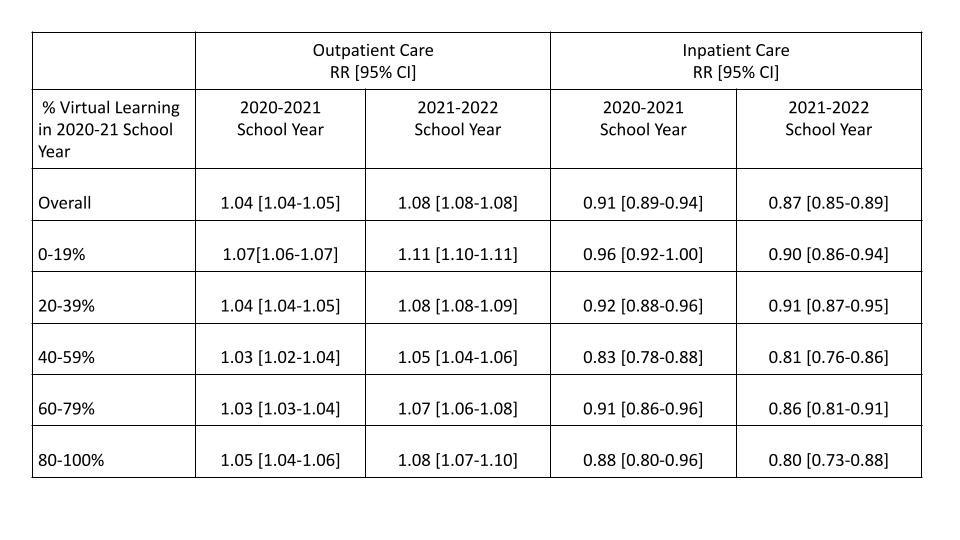
Results: A median of 1.4M children were included, the largest percentage of children lived in states with 20-39% VL in 2020-21, 49% were female, most had a parent of Senior Enlisted Rank, and most children were between the ages of 8-15 (Table 1). Over the full population of children, outpatient mental healthcare increased 4% in the 2020-21 school year, ranging from 3% in states with 40-79% VL to 7% in states with 0-19% VL. Inpatient mental healthcare decreased 9% for the population overall, ranging from a 17% decrease in states with 40-59% VL to 4% in states with 0-19% VL. In the 2021-2022 school year, overall outpatient mental healthcare increased 8%, ranging from 5% in states with 40-59% VL to 11% in states with 0-19% VL. Inpatient care decreased 13% overall, ranging from 20% in states with 80-100% VL to 9% in states with 0-19% VL (Table 2).
Conclusion(s): Results indicate increased but modest outpatient mental health needs of children and youth in 2020-21 and 2021-22 as compared with 2018-19. Results may suggest cumulative stress, but do not suggest a dose effect of VL. Decreased inpatient care may suggest less severe mental healthcare need, or changes in the healthcare landscape impacting access. Additional work must account for the impact of pre-pandemic care disparities.
.jpg)