Medical Education: Diversity, Equity & Inclusion
Medical Education 4: Diversity, Equity, & Inclusion 1
499 - Designing A Language Barriers Curriculum Using An Educational Framework
Publication Number: 499.125

Aunum Akhter, MD (she/her/hers)
Perinatal-Neonatal Fellow
University of Michigan
Ann Arbor, Michigan, United States
Presenting Author(s)
Background:
Language barriers are associated with unequal access to healthcare and poor patient outcomes due to communication gaps. These barriers are especially challenging in the Neonatal Intensive Care Unit given the acuity, chronic illnesses, and long-term follow-up associated with prematurity. Currently, there is no standard curriculum that educates neonatology medical learners about these barriers and how to address them. An established theoretical framework, such as the Six Steps of Medical Education Curriculum Development by Kern et al, aids in the creation of comprehensive objectives, promotes learner engagement, and lends itself to innovative educational tools and methods.
Objective:
To design an educational curriculum for neonatal-perinatal fellows (NPF) that addresses language barriers and best practices using interpretive services based upon the Six Steps of Medical Education Curriculum Development by Kern et al. (Step 1)
Design/Methods:
An anonymous web-based needs assessment was distributed to NPF and early career neonatologists via the American Academy of Pediatrics Training and Early Career Neonatologists listserv (Step 2). Program and individual learning objectives were designed based upon responses (Step 3). The objectives were matched with active learning methods (Step 4). Finally, an implementation plan (Step 5) and assessment tools (Step 6) were created to pilot the curriculum.
Results: The needs assessment identified that respondents infrequently use medical interpreters for daily patient updates compared to other clinical encounters (Table 1). Respondents who received formal education regarding interpreter services and cultural barriers among ethnic minorities had higher confidence scores using interpretive services compared to those who did not. Based on these findings, cognitive, psychomotor, process, and affective learning objectives were developed. A medical improvisation workshop was chosen as the best educational method because it provides active, experiential learning with real-time feedback. Standard and adapted improvisation exercises paired with focused debriefings were designed and align with the objectives (Table 2). Pre- and post-assessment tools were created to evaluate individual learning and program outcomes.
Conclusion(s):
A theoretical framework provides a comprehensive structure to develop a medical curriculum that addresses communication gaps associated with language barriers. Medical improvisation focuses on foundational communication skills and self-reflection which are essential in medicine. This workshop is undergoing pilot testing to assess learning outcomes. 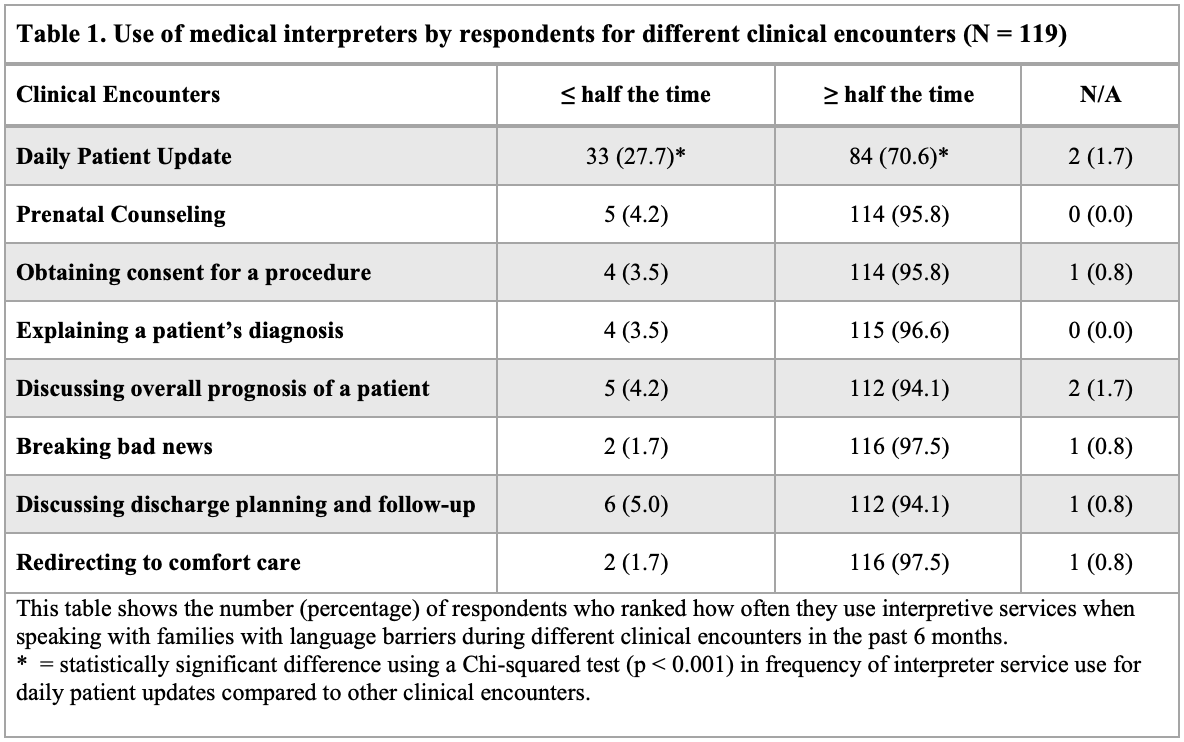
.png)
