Obesity
Obesity 1
388 - Caregiver Perspectives on Use of Telemedicine in an Urban Pediatric Obesity Clinic
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 388
Publication Number: 388.145
Publication Number: 388.145
Sara Malina, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Aditi Vasan, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Lorraine Katz, Childrens Hospital of Philadelphia, philadelphia, PA, United States; Rachana Shah, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Talia A.. Hitt, Johns Hopkins University School of Medicine, Lutherville-Timonium, MD, United States
- SM
Sara Malina, BA (she/her/hers)
Research Program Coordinator
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background: Pediatric obesity rates have increased rapidly over the past decade, particularly among children living in poverty. Telemedicine may be an effective way to reach low-income children and families with transportation barriers, but few studies have evaluated the acceptability of telemedicine for pediatric obesity care in urban settings.
Objective: Our study aimed to explore caregiver perceptions of and experiences with telemedicine for the management of pediatric obesity in an urban setting.
Design/Methods: An electronic survey with multiple-choice and free-text components was sent to all patients seen at a large academic urban pediatric obesity clinic from 4/21/21-5/12/21. Data were analyzed using descriptive statistics, and proportions were compared using Fisher’s exact test.
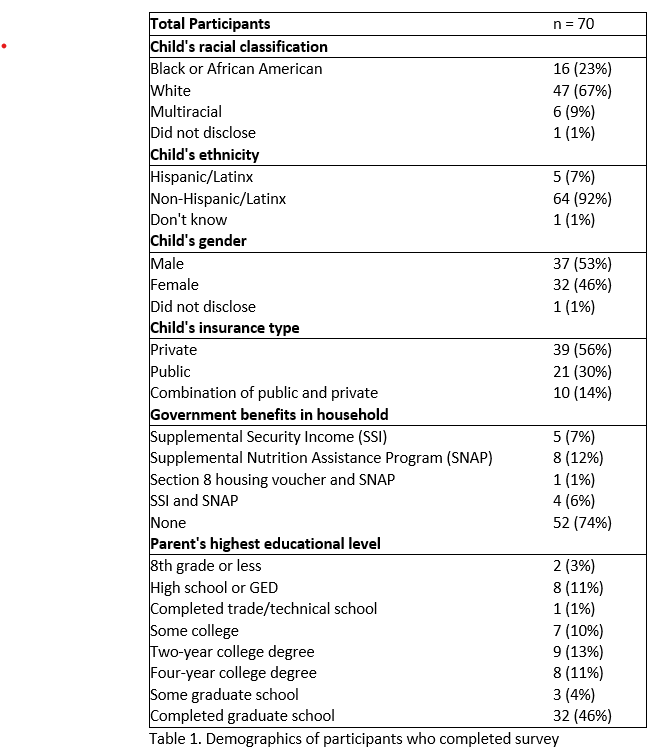
Results: 70 participants (4% response rate) completed the survey. 44% of caregivers had children who were publicly insured, 26% received other government benefits, and 39% were Black, Hispanic/Latinx, or multi-racial. Participants overwhelmingly reported having a phone (100%) or computer (97%) with internet access. Of patients who were offered video telemedicine appointments, 84% chose to have a telemedicine appointment, and 72% of those who had telemedicine appointments had more than one. Caregivers’ most common reason for choosing telemedicine was convenience, both in terms of scheduling and transportation. The most common reason cited for not choosing telemedicine was that the caregiver did not think it would be as helpful as an in-person visit. No caregivers indicated that lack of internet access was a reason for not choosing telemedicine. Of patients who had telemedicine visits, only 17% reported having technical difficulties. 57% of patients reported that there were no aspects of in person visits that they missed when switching to telemedicine. The most common visit components that participants missed were in-person interaction with providers, weigh-ins, working with an exercise physiologist in-person, and using gym equipment. Caregivers who chose telemedicine as opposed to in person visits did not show significant differences based on caregiver education level or on child race, ethnicity, or insurance status.
Conclusion(s): Telemedicine video visits are a well-accepted and convenient tool for reaching pediatric obesity patients in an urban setting. Urban pediatric obesity clinics should offer caregivers the option of telemedicine visits to improve access to care, and payers should adopt reimbursement models that support the use of telemedicine for pediatric obesity care.