Obesity
Obesity 2
408 - Weight Status and Social Factors Among Emerging Adults in the National Health Interview Survey, 2009-2018
Publication Number: 408.146

Alejandra Ellison-Barnes, MD, MPH
Assistant Professor
Johns Hopkins University
Baltimore, Maryland, United States
Presenting Author(s)
Background:
Little research has explored the relationship between social determinants and obesity in emerging adulthood, the unique developmental period from ages 18-25, despite the importance of this period in establishing habits and lifestyle that may persist throughout adulthood and contribute to an individual’s long-term weight and health trajectories.
Objective: Our objective was to describe the relationship between social factors and weight status in a large, nationally representative sample of emerging adults.
Design/Methods:
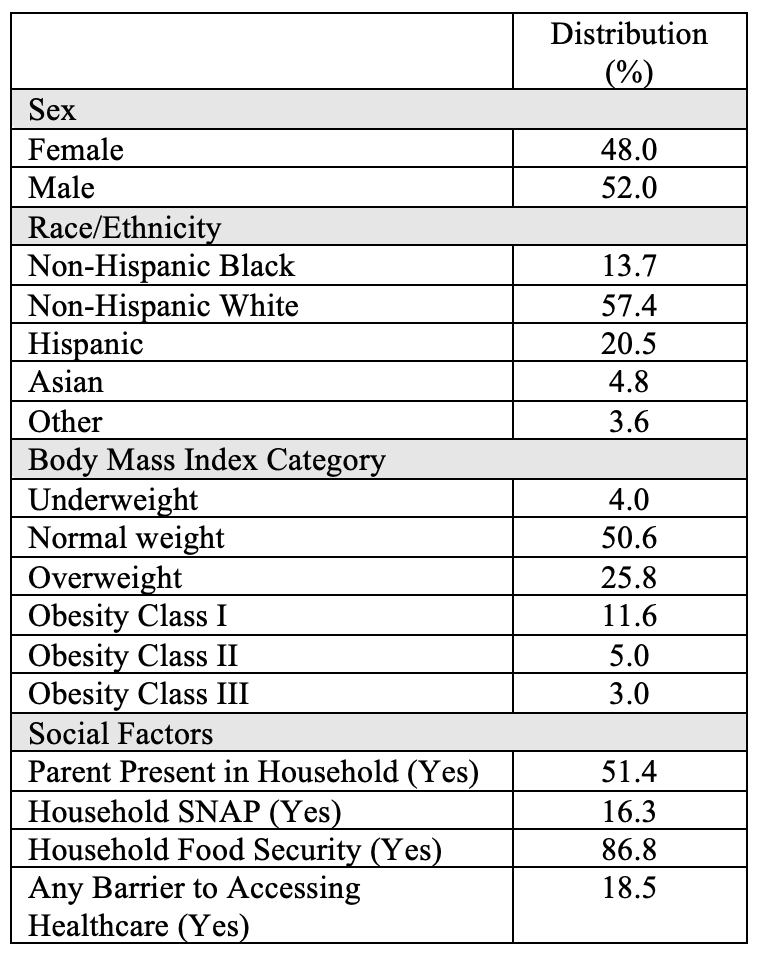
We used data from the National Health Interview Survey (NHIS) years 2009-2018, including emerging adults aged 18-25. Survey weights were used to account for complex survey design. We used descriptive statistics to evaluate the distribution of weight status and selected social factors. Weight status was classified based on body mass index (BMI) as underweight (BMI < 18.5 kg/m2), normal weight (BMI 18.5-24.9 kg/m2), overweight (BMI 25-29.9 kg/m2), class I obesity (BMI 30-34.9 kg/m2), class II obesity (BMI 35-39.9 kg/m2), and class III obesity (BMI ≥40 kg/m2). Social factors included parental presence in household (proxy for living with parent(s)), household receipt of Supplemental Nutrition Assistance Program (SNAP) benefits, household food insecurity, and barriers to accessing healthcare (for example, limited office hours or lack of transportation). We conducted a bivariate analysis exploring the relationship between social factors and BMI.
Results:
We included 32,443 emerging adults; Table I shows the overall distribution of demographics, weight status, and social factors. In bivariate analyses, higher mean BMI was significantly associated with household receipt of SNAP (27.3 kg/m2 vs 25.4 kg/m2, p< 0.0001), household food insecurity (26.9 kg/m2 vs 25.4 kg/m2, p< 0.0001), and having any barrier to healthcare access (26.4 kg/m2 vs 25.6 kg/m2, p< 0.0001). There was no significant difference in mean BMI by parental presence.
Conclusion(s):
Several social factors were associated with higher mean BMI among a national sample of emerging adults, which is similar to prior observations in children. Adjusted analyses accounting for key covariates such as sex, race/ethnicity, physical activity, smoking status, and survey year are underway. These findings may inform future interventions at the individual, community, and policy levels to prevent and treat obesity during emerging adulthood, potentially yielding lifelong reductions in obesity-related morbidity and mortality.