Hospital Medicine: Hospital Medicine Quality Improvement
Hospital Medicine 1
747 - Improving Patient Flow Through Discharge Efficiency
Publication Number: 747.119
.jpeg.jpg)
Meghan W. Harrison, MD
Pediatric Hospital Medicine Fellow
University of Alabama at Birmingham
Vestavia, Alabama, United States
Presenting Author(s)
Background:
The recent respiratory viral surges affecting children’s hospitals have highlighted a vulnerability to care: inpatient capacity. To meet this challenge, we looked to smooth patient flow from admission to discharge. A key bottleneck identified was afternoon discharge clustering. We sought to improve timeliness of discharge based on patient medical readiness.
Objective:
Increase the percentage of monthly discharges from the acute care unit during nonpeak hours (5pm – 11am) from 29% to 44% (a 50% increase from baseline) by June of 2023.
Design/Methods: An interdisciplinary throughput committee was established to study the discharge process. This committee consists of hospital administrators, nurses, physicians, social workers, case managers, and environmental services staff. Baseline data were obtained from January 2020 to December of 2021 to determine peak discharge hours. A key driver diagram (Figure 1) was created. The primary outcome of this initiative is percent of “nonpeak” discharges that occur between 5pm and 11am. Secondary outcome of average length of stay (LOS) and balancing measure of hospital readmission rate were also studied. The primary interventions include: earlier physician rounding times, creation of standardized discharge criteria for five of the most common admission diagnoses, and direct physician discharge performance feedback. We meet bimonthly to review progress and consider further interventions using Plan-Do-Study-Act (PDSA) cycles.
Results:
Baseline data revealed that a majority of discharges (71%, n=6536) were occurring during the hours of 11am and 5pm. Since initiation of interventions in May of 2022, the mean percentage of nonpeak hour discharges has increased from 29% to 35%, a 22% increase from the baseline (Figure 2). Importantly, targeting physician rounding practices by encouraging discharge of medically ready patients before rounds has lead to an increase in discharges before 11am (13.7% to 20.9%) since June of 2022. Average LOS has not shown significant improvement, and balancing measure data is still being collected.
Conclusion(s):
Our project demonstrated that throughput efficiency can be improved with selected interventions. The team has increased the percent of patients that are specifically discharged before 11 am, leading to faster bed turnover for admissions and transfers and decreased boarding in the emergency department. Reinforcement of standardized discharge criteria through the electronic medical record and expansion of interventions across service lines are future next steps.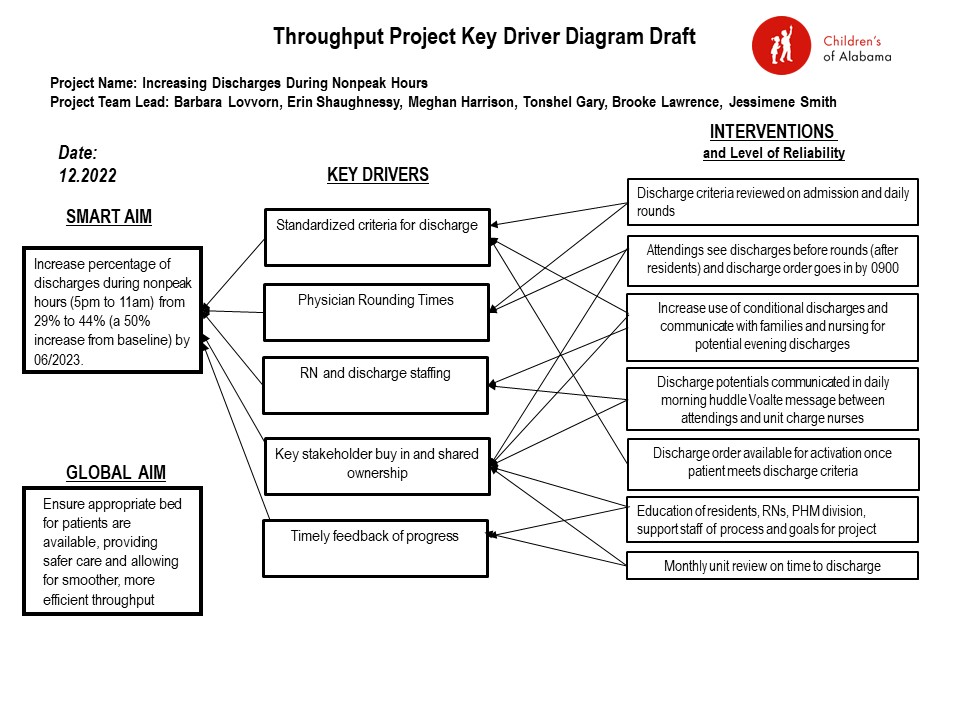
.jpg)
