Hospital Medicine: Hospital Medicine Quality Improvement
Hospital Medicine 1
743 - Addressing Social Needs in the Hospital Has a Lasting Impact: A Quality Improvement Project to Optimize Inpatient Food and Diaper Insecurity Screening and Mitigation
Publication Number: 743.119

Amy S. Buczkowski, MD (she/her/hers)
Assistant Professor of Pediatrics, Hospitalist Attending
The Barbara Bush Children's Hospital at Maine Medical Center
Portland, Maine, United States
Presenting Author(s)
Background:
Social determinants of health are drivers of pediatric health outcomes. For example, food insecurity in children is associated with higher hospitalization risk and poorer health. Screening is helpful in identifying and addressing social needs, and evidence supports inpatient social needs screening.
Objective:
This inpatient quality improvement project aimed to implement a universal process to identify patients with food and/or diaper insecurity and improve inpatient social need mitigation.
Design/Methods:
A team of nurses (RN), physicians, and social workers (SW) on a 30-bed pediatric inpatient unit created a food and diaper insecurity screening and mitigation workflow and used Model for Improvement methodology to work towards our aims. Screening via questionnaire was done by RNs and transcribed into the electronic health record (EHR). A workflow for patients identified with food and/or diaper insecurity included an automatic EHR alert for SW consult order, community resources referral, and emergency food or diaper provision if needed. Data were collected via retrospective chart review and phone calls to caregivers of patients with positive screens. Process measures included food and diaper insecurity screening rates and SW consult order placement rate for patients with positive screens. Outcome measure was the percentage of families that used or planned to use referred community resources. The balance measure was the percentage of families comfortable with and supportive of inpatient social needs screening.
Results:
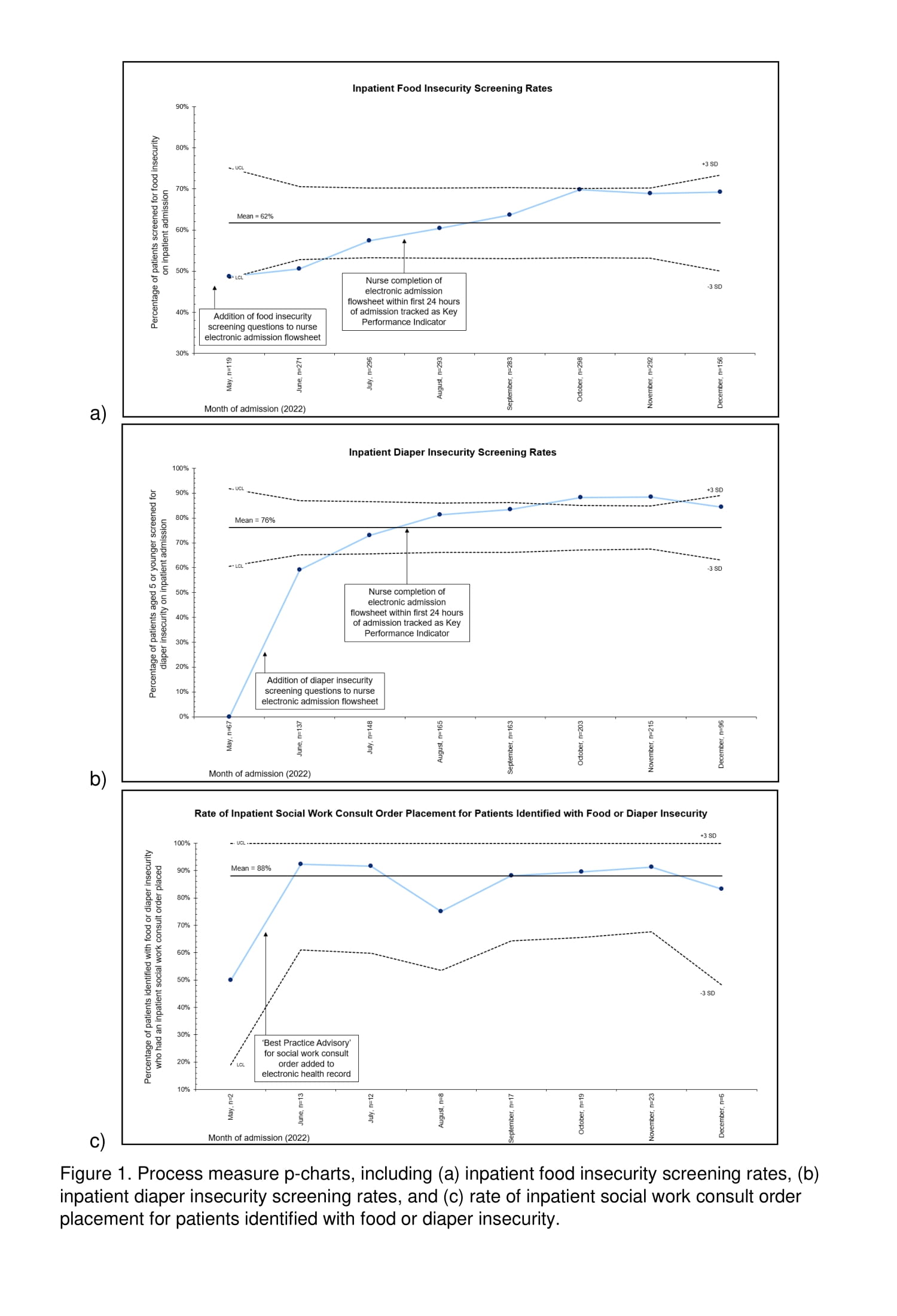
Average food and diaper insecurity rates in our population were 6% and 7%, respectively. Between May and November of 2022, food and diaper insecurity screening rates increased from 49% to 69% and 59% to 88%, respectively. SW consult orders placed for patients with positive screens improved (50% to 91%) (Figure 1). For caregivers of patients connected with community resources, 75-100% used or planned to use the resources. Caregivers of patients with positive screens felt comfortable being asked the screening questions and supportive of inpatient social needs screening 80-100% of the time.
Conclusion(s): By creating a combined inpatient food and diaper insecurity screening process, we were able to identify patients with food and/or diaper insecurity and connect the identified patients with resources in a comfortable manner for families. Families who received resource referrals were likely to have used or planned to use the community resources, which suggests these interventions may improve a patient's access to food and/or diapers following discharge.