Emergency Medicine: All Areas
Emergency Medicine 2
38 - Performance of the Asthma Clinical Score in the evaluation of acute asthma exacerbations in the emergency department
Publication Number: 38.111

Adjoa A. Andoh, MD (she/her/hers)
Assistant Professor, Pediatrics, Division of Emergency Medicine
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background:
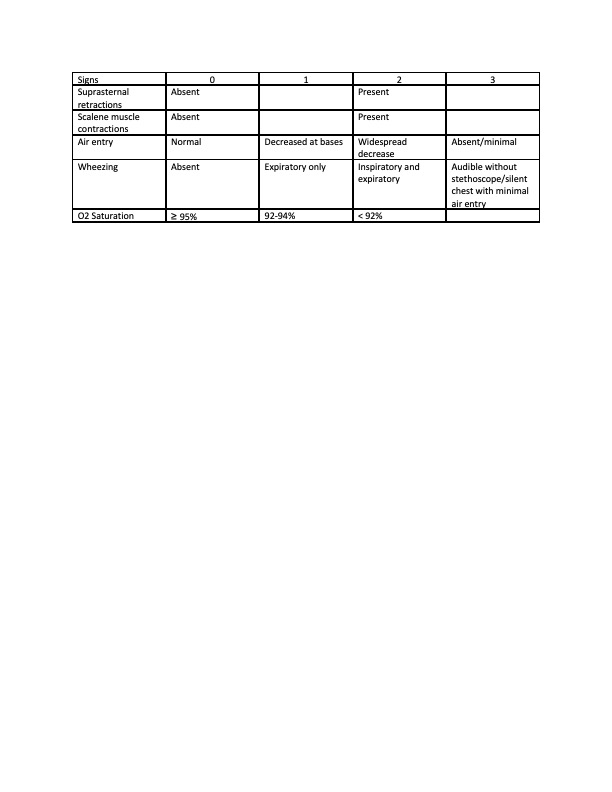
Management of acute asthma exacerbations in the emergency department (ED) is based off assessment of severity. Various scores were developed to objectively assess severity. The Asthma Clinical Score (ACS) (Table 1), developed for use in guiding inpatient albuterol administration, was introduced as part of an ED clinical pathway to guide acute asthma management. It has not been formally validated in this setting.
Objective:
The primary objective of this study is to compare the performance of the ACS to the Pediatric Respiratory Assessment Measure (PRAM) (Table 2), a validated asthma severity score. Our secondary objectives are to determine ACS interrater reliability, predictive validity, and responsiveness.
Design/Methods:
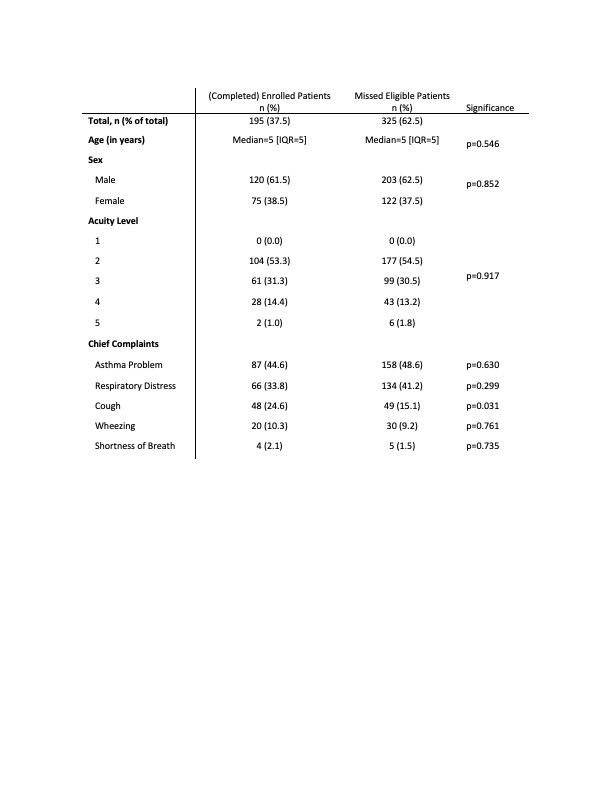
This is a single site prospective observational study of children ages 2-17 years presenting to the ED for asthma exacerbations. Children with bronchiolitis, co-morbid conditions, or chronic lung diseases are excluded. Physicians, nurses, and respiratory therapists complete electronic based forms of paired assessments of patients using the PRAM and ACS at three points: initial presentation, after completion of first treatment, and ED disposition. Demographics of enrolled and missed eligible patients will be compared using Wilcoxon rank sum test and Fisher’s exact test as appropriate. Construct validity comparing the performance of the ACS to the PRAM, interrater reliability, predictive validity for patient disposition and responsiveness to detect change in clinical status will be analyzed using Spearmen’s correlation coefficient, Cohen’s kappa coefficient, area under receiver operating characteristics (AUROC) and paired t-test respectively. To detect a difference between the null hypothesis correlation of 0.8 and alternative hypothesis of 0.85 with sufficient power at a 0.05 significance level, 320 subjects will be enrolled. Data collection is ongoing.
Results:
To date, we have enrolled 195 children. Patient demographics are listed in Table 3. In this interim analysis, ACS and PRAM were strongly associated with each other at all time points [p=0.877, 95% CI=(0.86, 0.89)]. ACS showed strong interrater reliability at all timepoints (k=0.83). First ACS was a very good predictor of hospital admission [AUROC=0.79, 95% CI=(0.70, 0.85)]. In terms of responsiveness, there was a 2.9-point difference in ACS from first assessment to disposition (p value< 0.0001).
Conclusion(s):
ACS performed comparably to PRAM and was a reliable and valid score with good predictive properties in this cohort. This study supports the ACS as a useful tool in ED assessment of asthma exacerbation severity in children..jpg)