Critical Care
Critical Care 1
6 - Consistent ventilator management for infants with congenital diaphragmatic hernia improves outcomes
Publication Number: 6.107

Katrin Lichtsinn, MD (she/her/hers)
Fellow Physician
UPMC Childrens Hospital of Pittsburgh
Pittsburgh, Pennsylvania, United States
Presenting Author(s)
Background: Lung hypoplasia and pulmonary hypertension contribute to morbidity and mortality in infants with congenital diaphragmatic hernia (CDH). Respiratory management optimizing lung recruitment while minimizing injury improves outcomes. In January 2012 our NICU implemented a standardized clinical practice guideline (CPG) to manage infants with CDH, which led to improved survival and decreased ECMO use. The CPG emphasized consistent respiratory management by maintaining goal ventilator and blood gas parameters.
Objective: Determine differences in ventilator management before and after CPG implementation.
Design/Methods:
Retrospective study of infants with CDH admitted from January 2007 to July 2021. Pre-CPG (2007-2011) and post-CPG (2012-2021) cohorts were studied. Infants with Morgagni hernia, intubated < 24 hours, on ECMO < 24 hours of admission or first intubated >14 days of life were excluded. Demographic data, ventilator settings and blood gasses at 0 and 24 hours of mechanical ventilation, and hourly ventilator setting ranges (within or outside CPG goal parameters) for the first 7 days of mechanical ventilation or until ECMO were abstracted. The cohorts were compared with descriptive statistics.
Results:
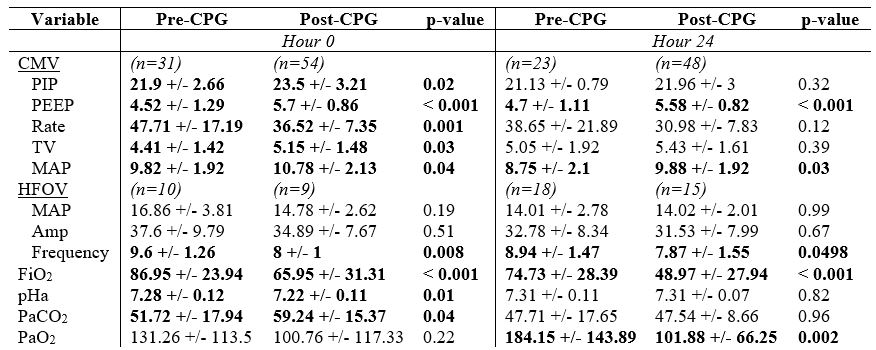
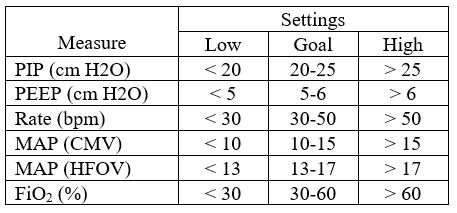
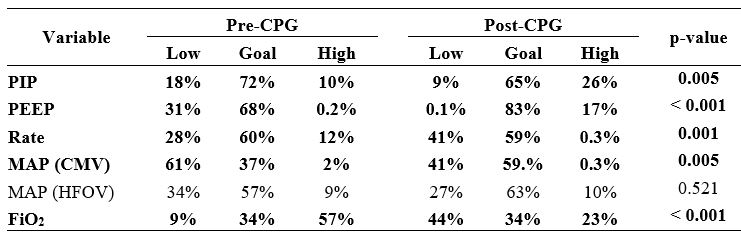
104 infants met inclusion criteria; 41 pre-CPG and 63 post-CPG. There were no significant demographic differences between cohorts. Post-CPG, ECMO use decreased (39% vs 11%, p=0.001), overall survival increased (66% vs 92%, p=0.001), and survival for ECMO patients increased (31% vs 100%, p=0.005). Overall, post-CPG cohort spent more time on conventional mechanical ventilation (CMV) vs high-frequency oscillatory ventilation (HFOV; p< 0.001). At 0h, CMV use was similar in both cohorts (76% vs 86%) but post-CPG significantly more patients remained on CMV at 24h (56% vs 76%, p=0.03). At 0h, post-CPG cohort had higher PIP, PEEP, tidal volume, and CMV-MAP but lower rate and FiO2 (Table 1). By 24h, post-CPG cohort still had higher PEEP and MAP with even lower FiO2. Post-CPG cohort had more acidosis and hypercarbia at 0h (corrected at 24h), while pre-CPG cohort had significantly higher PaO2 by 24h. Median percent time spent in low, goal, or high ventilator settings for PIP, PEEP, rate, CMV-MAP, and FiO2 were significantly different between cohorts over the first 7 days of ventilation; post-CPG cohort maintained higher PIP and PEEP with lower rate and FiO2 (Tables 2, 3).
Conclusion(s):
Consistent ventilation management for infants with CDH that employs optimal pressures to maintain adequate lung expansion and avoid atelectrauma while also minimizing oxygen toxicity may reduce ECMO utilization and improve outcomes.