Hospital Medicine: Hospital Medicine Quality Improvement
Hospital Medicine 1
744 - Barriers, Facilitators, and Time Costs of Implementing a High-Efficiency Pediatric Clinical Pathway Intervention: A National, Mixed-Methods Study
Publication Number: 744.119

Sara M. Aziz, MD (she/her/hers)
Pediatric Hospital Medicine Fellow
University of California, San Francisco, School of Medicine
San Francisco, California, United States
Presenting Author(s)
Background: Clinical pathways are simple, visual diagrams that guide clinicians step-by-step through the evidence-based care of a specific medical condition. Time costs of pathway implementation are poorly understood, and these quality improvement (QI) efforts are often under-resourced and tasked to women and/or underrepresented groups. The SIP trial (Simultaneously Implementing Pathways for Improving Asthma, Pneumonia, and Bronchiolitis Care for Hospitalized Children) is a national, hybrid implementation-effectiveness trial of a high-efficiency pathway intervention.
Objective: Our objective in this study is to describe implementation fidelity (use of implementation strategies as intended), time costs, barriers, and facilitators in a national sample of community children’s hospitals.
Design/Methods:
We conducted a mixed-methods study of hospitals participating in the ongoing SIP trial. Hospitals received pathways and used 5 implementation strategies: meetings with external QI mentors/facilitators, educational sessions, Plan-Do-Study-Act (PDSA) cycles, audit and feedback, and clinical decision support via electronic order sets. Data was collected through monthly surveys of physician site leaders. Quantitative data was analyzed using descriptive statistics, and qualitative data was analyzed using thematic content analysis.
Results:
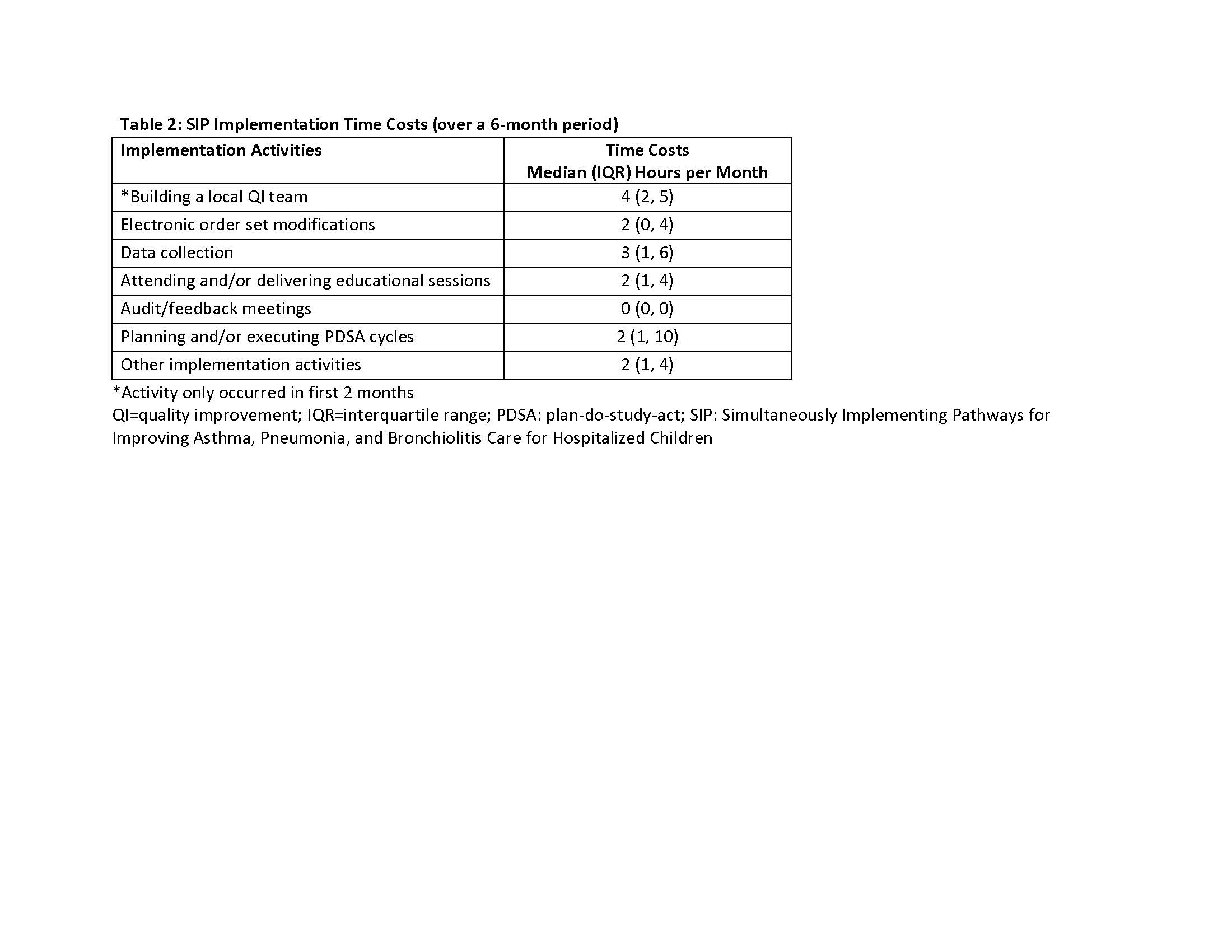
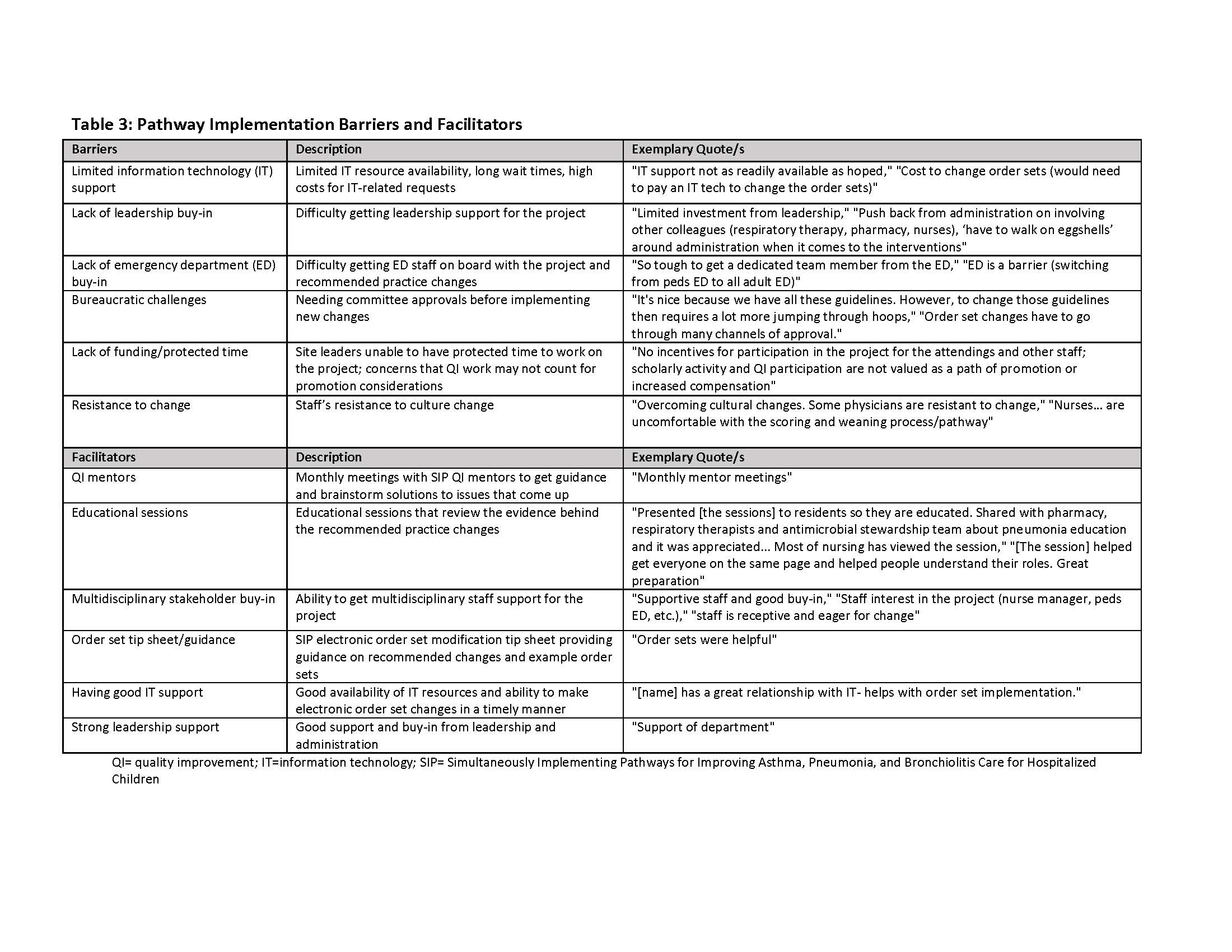
Twenty site leaders (from 20 hospitals) and 8 QI mentors participated. Monthly surveys examined implementation activities over 6-months, and completion rates ranged from 70-90%. Implementation fidelity is described in Table 1. Strategies with the highest fidelity were educational sessions and QI mentor meetings; those with lowest fidelity were audit and feedback and electronic order set modifications. Implementation time costs are described in Table 2. Data collection had the highest time cost. Most frequently reported barriers and facilitators of implementation are outlined in Table 3. Common barriers included limited information technology support and lack of leadership buy-in. Facilitators included QI mentors and educational resources.
Conclusion(s):
Our study provides detailed guidance on implementation fidelity, time costs, barriers, and facilitators for hospitals seeking to improve pediatric care quality through clinical pathway implementation. Quantifying the time costs of these efforts is critical to improving future resource allocation..jpg)