Medical Education: Resident
Medical Education 1: Resident 1
452 - A Need for Time and Training: Pediatric Program Directors' Perceptions about Mentorship
Publication Number: 452.122

Margaret Shope (she/her/hers)
Medical Student
University of Chicago Division of the Biological Sciences The Pritzker School of Medicine
Chicago, Illinois, United States
Presenting Author(s)
Background:
Mentorship benefits medical trainees and institutions, and the Accreditation Council for Graduate Medical Education (ACGME) requires mentorship in pediatric residencies. A national survey evaluating mentorship in pediatric residency programs has yet to be conducted.
Objective:
We aimed to describe existing mentorship programs in pediatric residencies, assess whether mentorship program characteristics impact mentoring outcomes, and identify barriers to mentorship program success.
Design/Methods:
With support from the Association for Pediatric Program Directors (APPD) Research Task Force, we conducted a cross-sectional study of associate pediatric program directors (APDs) in the United States. Results were analyzed using descriptive statistics, univariate logistic regression, and thematic analysis of open-ended questions.
Results:
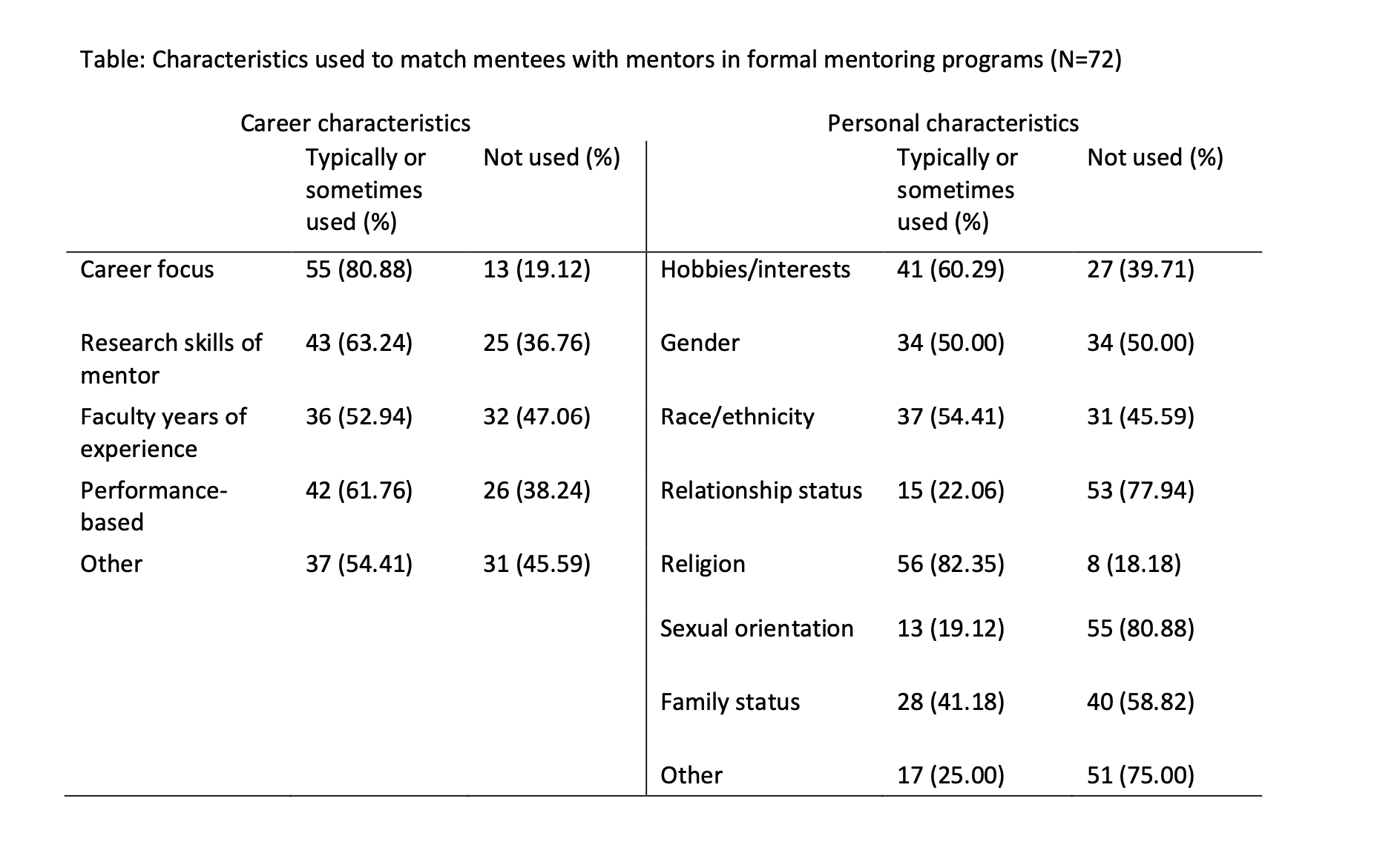
82 of 197 (41.6%) programs responded. There was no significant difference in response rate by program or region. 87.8% report having a formal mentoring program. Most leaders were at least “mostly satisfied” (63.4%) with their mentorship program, and perceive residents (57.4%) and faculty (68.3%) as least “mostly satisfied.” Of those with formal programs, 80.6% assign mentorship pairs through the program director, and 57.4% solicit resident pairing preferences. Career characteristics are more commonly used for pairing than personal characteristics. Most programs (80.6%) do not protect faculty time spent on mentorship. Half of programs (51.4%) do not provide mentee training to residents, and 37.5% do not train faculty mentors. Faculty lacking time is a top barrier for 86.1% of programs. Other commonly cited top barriers include residents lacking time (40.3%) and inadequate funding (22.2%). Training of mentees is associated with increased program leader satisfaction, OR 3.2 (95% CI 1.1-9.4, p = .03).
Conclusion(s): Most pediatric residencies have a formal mentorship program. Strategies for pairing, including soliciting resident preference, vary across programs. Though mentor-mentee identity concordance is perceived as beneficial by mentees, especially women and those underrepresented in medicine, career characteristics are more often used for pairing than personal characteristics. A lack of funding and lack of ability to protect faculty and resident time were cited as major barriers to mentorship efforts. National organizations, such as APPD and the ACGME, have an opportunity to provide guidance and support for protected time, funding, and training, and more research is called for to investigate the mentor and mentee perspective on formal mentorship in their programs.