Injury Prevention
Injury Prevention 1
132 - Assessing the impact of a helmet distribution program in the pediatric emergency department
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 132
Publication Number: 132.121
Publication Number: 132.121
Nicolas Delacruz, Hassenfeld Children's Hospital at NYU Langone, Long Island City, NY, United States; Kathryn Varghese, CUNY School of Medicine, New York, NY, United States; Allan B.. Pulliam, Texas A&M Health Science Center College of Medicine, Austin, TX, United States; Angelica Almader-Ruiz, New York University Grossman School of Medicine, New York, NY, United States; Ee Tay, NYU School of Medicine, New York, NY, United States

Nicolas Delacruz, MD (he/him/his)
Fellow
Hassenfeld Children's Hospital at NYU Langone
Long Island City, New York, United States
Presenting Author(s)
Background: Cycling and the use of other non-motorized wheeled vehicles such as skateboards and scooters are becoming increasingly popular modes of transportation and recreation in The United States. Helmet use is one of the simplest and most effective methods of protecting riders from injury. Despite overwhelming data to support their role in reducing injury, a majority of young children and adolescents still do not regularly wear helmets.
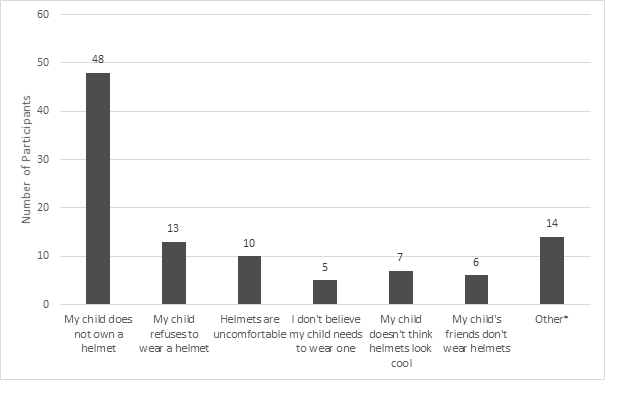
Objective: Our primary objective was to determine if a simple, Emergency Department (ED)-based helmet distribution program can increase the amount of time children self-report wearing helmets. Our secondary objective was to define common reasons why children may not wear helmets.
Design/Methods: This was a prospective cohort study of children aged 2-17 years presenting to the ED of an urban, tertiary care hospital with any chief complaint. Enrollment took place on nonconsecutive days from May to October, 2022. Participants were given a likert scale-based survey asking about their helmet use habits and their perceptions regarding the efficacy and importance of helmets. Participants then received a bicycle helmet along with bicycle safety handouts provided by the American Academy of Pediatrics. Participants were contacted by researchers 2 months after enrollment to complete a follow up survey regarding helmet wearing habits after helmet distribution.
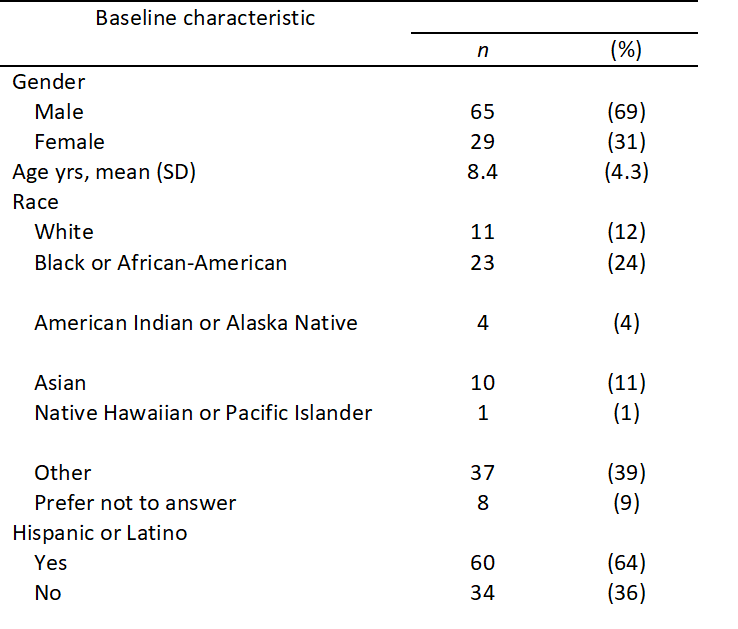
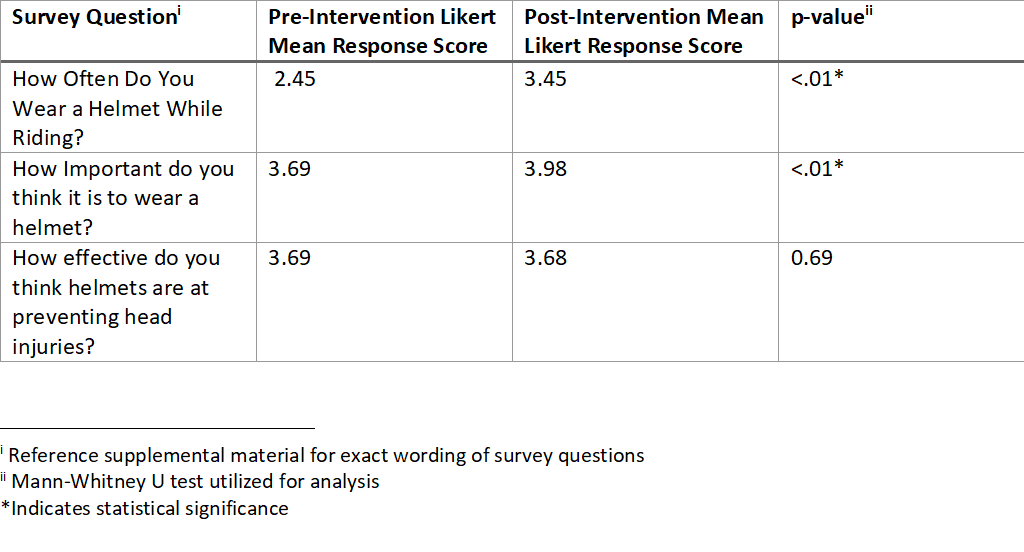
Results: A total of 94 patients were enrolled in the study (Table 1). The most popular wheeled vehicle used by participants were bicycles. Post-intervention surveys were obtained from 44 (47%) patients and their families. Receiving a bicycle helmet and brief counseling in the ED resulted in a statistically significant increase in the amount of time children reported wearing bicycle helmets (Table 2). Prior to ED intervention, 48% of participants reported wearing a helmet “most of the time” or “all of the time”. After a helmet was distributed, 86% of participants indicated that they wore a helmet “most of the time” or “all of the time” while riding wheeled vehicles. Despite low rates of pre-intervention helmet use, 91% of patients indicated that wearing a helmet was “moderately or extremely important”. Participants indicated a variety of reasons for not wearing helmets (Figure 1). 16% of patients indicated on follow-up surveys that their helmets prevented a head injury.
Conclusion(s): Helmet distribution programs based in urban, pediatric emergency departments are simple and effective ways to increase rates of bicycle helmet usage amongst pediatric patients. Additional research is needed to determine impact on head injury prevention.