Medical Education: Diversity, Equity & Inclusion
Medical Education 4: Diversity, Equity, & Inclusion 1
504 - Improving Awareness of Offensive Terms in Medicine Through the Lens of Vancomycin Infusion Reaction
Publication Number: 504.125

Steven Ham, MD, MPH (he/him/his)
Resident Physician
Cohen Children's Medical Center at Northwell Health
Roslyn, New York, United States
Presenting Author(s)
Background:
Curricula on American Indian/Alaska Native (AI/AN) health are lacking in the American medical education system. Understanding historical trauma and social determinants of health for AI/AN children is crucial to achieving equitable care. It is established that biases are pervasive in medicine and offensive or stigmatizing language are examples of how bias perpetuates.
Objective:
To improve awareness of AI/AN health disparities and increase awareness of offensive terms in medicine like “Red Man Syndrome” (RMS).
Design/Methods:
This was a single institution study at a pediatrics residency program. The intervention was a 6.5-minute video outlining AI/AN health inequities and historical traumas to highlight the racially insensitive and inaccurate term RMS. This was followed by preferred terms to replace other micro-aggressive terms or eponyms for violators of human rights. Residents completed pre- and post-intervention (immediately, 3-months, and 6-months) Likert scale surveys, with analyses conducted by Wilcoxon signed rank tests. Also, a free response question asked participants to name the phenomenon when a patient develops diffuse erythema after vancomycin infusion with analysis performed via Chi-squared test. An alpha value of 0.01 was used for statistical significance. Statistical analyses were performed with R (v4.2.2) and R Studio (v2022.12.0-353).
Results:
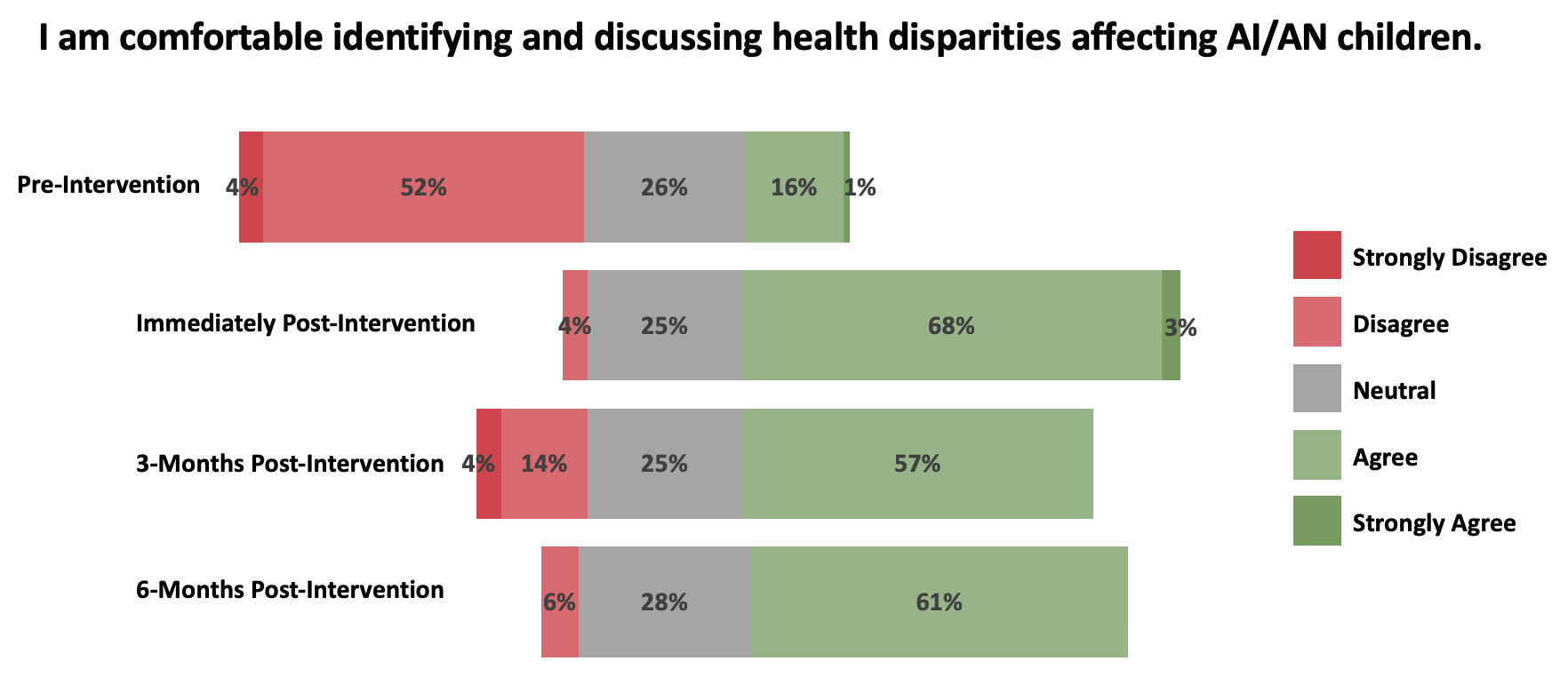
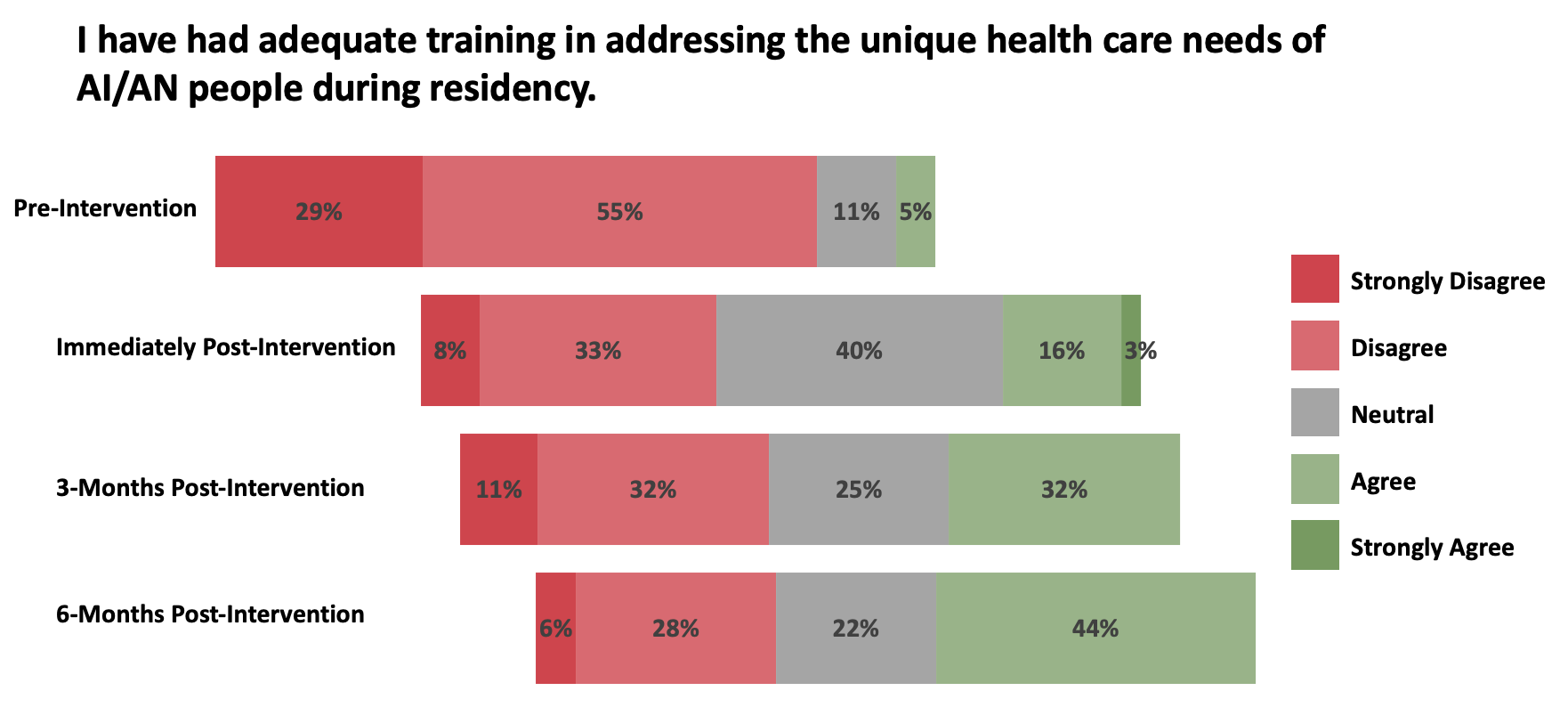
73 residents participated with all completing the immediate, 28 completing the 3-months, and 18 completing the 6-months post-intervention surveys. There were significant changes in residents’ comfort discussing health disparities affecting AI/AN children (p-value < 0.001 at all time points), perceived adequacy of training in residency to address the health care needs of AI/AN people (p-value < 0.001 at all time points), comfort addressing racist micro-aggressive behaviors in medicine (p-value < 0.001 immediately and 3-months post-intervention), and comfort identifying other offensive terms in medicine (p-value < 0.001 immediately and 3-months post-intervention). The intervention also had a significant effect (p-value < 0.001) on residents’ response to our free response prompt immediately post-intervention; moreover, 28/28 and 18/18 residents responded with “vancomycin infusion reaction” at the 3-month and 6-month post-intervention marks respectively.
Conclusion(s):
These results demonstrate a successful intervention for improving medical trainees’ awareness of offensive terms in medicine through the lens of AI/AN health inequities and the term RMS. Minimizing stigmatizing language in medicine is an essential step towards reducing bias in medicine.