Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 3
543 - COVID disruptions and parent well-being: Role of family resilience, functioning, and self-efficacy
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 543
Publication Number: 543.118
Publication Number: 543.118
Keith J. Martin, Johns Hopkins University School of Medicine, Baltimore, MD, United States; William Heerman, Vanderbilt University Medical Center, Nashville, TN, United States; H. Shonna Yin, NYU School of Medicine, New York, NY, United States; Lee M. Sanders, Stanford University, Stanford, CA, United States; Kori Flower, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, United States; Russell L. Rothman, Vanderbilt University School of Medicine, Nashville, TN, United States; Alan M. Delamater, University of Miami Leonard M. Miller School of Medicine, Miami, FL, United States; Charles T. Wood, Duke University, Durham, NC, United States; Jonathan S. Schildcrout, Vanderbilt University Medical Center, Nashville, TN, United States; Evan C. Sommer, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Michelle White, Duke University School of Medicine, Durham, NC, United States; Eliana M. Perrin, Johns Hopkins University School of Medicine, Baltimore, MD, United States

Keith J. Martin, DO, MS
Assistant Professor
Johns Hopkins University School of Medicine
Baltimore, Maryland, United States
Presenting Author(s)
Background: COVID-19’s negative impact on parent well-being has been widely reported, but little is known about potentially protective family-level factors that may mitigate this impact.
Objective: To examine whether the relationship between COVID-19 disruption and parent well-being was moderated by family resilience, family functioning, or parent COVID-related self-efficacy.
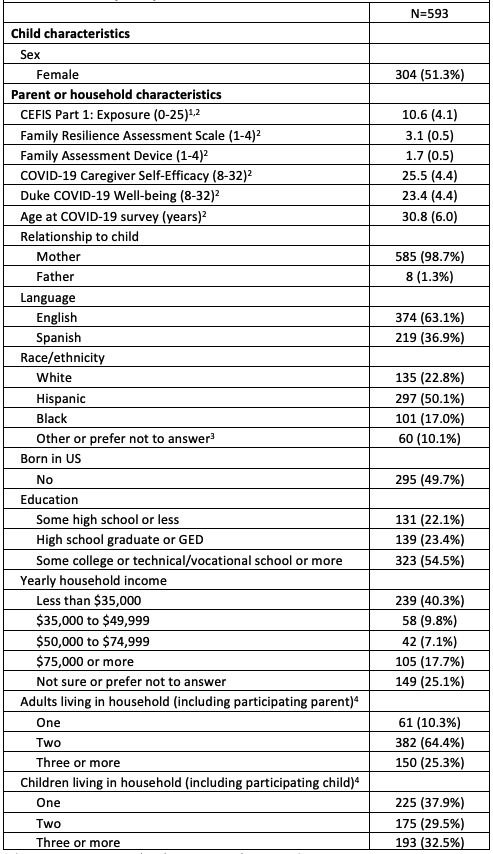
Design/Methods: A subset of parents of infants in an ongoing multi-site study completed additional COVID-19-related surveys, including measures of COVID-19 disruption (using the CEFIS Part 1: Exposure), parent well-being during the pandemic, family resilience, family functioning, and COVID-related self-efficacy. Three regression models assessed whether the association between disruption and well-being was moderated by resilience, functioning, or self-efficacy, after adjusting for covariates including: child and parent age as well as parent or household language, race/ethnicity, nativity, education, income, and number of adults and children in the household. Plots of model-based estimates show the disruption-well-being relationship for high and low moderator values.
Results: Out of 900 parents, 593 completed the full survey (17% Black, 50% Hispanic, 40% household income < $35k). The mean (SD) was 10.6 (4.1) for disruption (0-25 scale), and 23.3 (4.4) for well-being (8-32 scale; Table 1). Point estimates indicated that higher COVID-19 disruption was associated with lower well-being, but the association was only statistically significant in the family functioning model (-0.38; 95% CI=[-0.64, -0.13]; p=0.003). The interaction terms were not statistically significant in any model. However, family functioning (B=-3.92; 95% CI=[-5.61, -2.22]; p< 0.001) and self-efficacy (B=0.35; 95% CI=[0.15, 0.54]; p=0.001) were significantly associated with well-being, and the family resilience-well-being relationship was marginally significant (B=1.75; 95% CI=[-0.20, 3.70]; p=0.08). Results are plotted in Figure 1: for both high and low moderator values, as disruption increased, estimates of well-being appear to decrease, but the slopes of the lines appear nearly parallel (i.e., no meaningful interaction).
Conclusion(s): Associations between COVID-19 disruption and parent well-being were not moderated by family resilience, family functioning, and COVID-related self-efficacy in this sample of parents of infants. However, the observed associations between family resilience, family functioning, and COVID-related self-efficacy and parent well-being suggest an avenue for future research to determine appropriate intervention targets to improve parent well-being.
.jpg)
