Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 3
546 - Far from home: The impact of geographic distance from tertiary paediatric hospitals on family expenses and experiences
Publication Number: 546.118

Asia L. van Buuren, MD (she/her/hers)
Pediatrics Resident
University of British Columbia
Vancouver, British Columbia, Canada
Presenting Author(s)
Background:
Many children and their families living in rural and remote communities are required to travel to receive essential health care at tertiary pediatric hospitals in Canada. Despite this, there is a lack of available literature on their experiences, specifically associated costs and psychosocial impacts.
Objective: 1) Analyze administrative data to quantify the number of admissions and length of stay for families living > 50 km from a tertiary pediatric hospital in Canada.
2) Describe the costs and psychosocial impacts of hospitalization for these families.
Design/Methods:
Ethics approval was obtained. Family partners were involved in all aspects of study design. We obtained a de-identified data set describing the length of stay and home community of pediatric patients admitted to our clinical teaching unit (CTU). A cross-sectional survey was distributed to interested caregivers admitted to CTU. The survey included optional questions to assess participant demographics, costs associated with hospitalization, and subjective stress levels. Descriptive statistics were reported to address the study objectives.
Results:
Administrative data analysis described 2,759 admissions to CTU in 2021. Patients from communities > 50 km from the tertiary pediatric hospital were 22.5% of admissions. There was a strong statistical relationship between length of stay and distance from the tertiary centre (Pearson chi2 coefficient 90.1, p < 0.001).
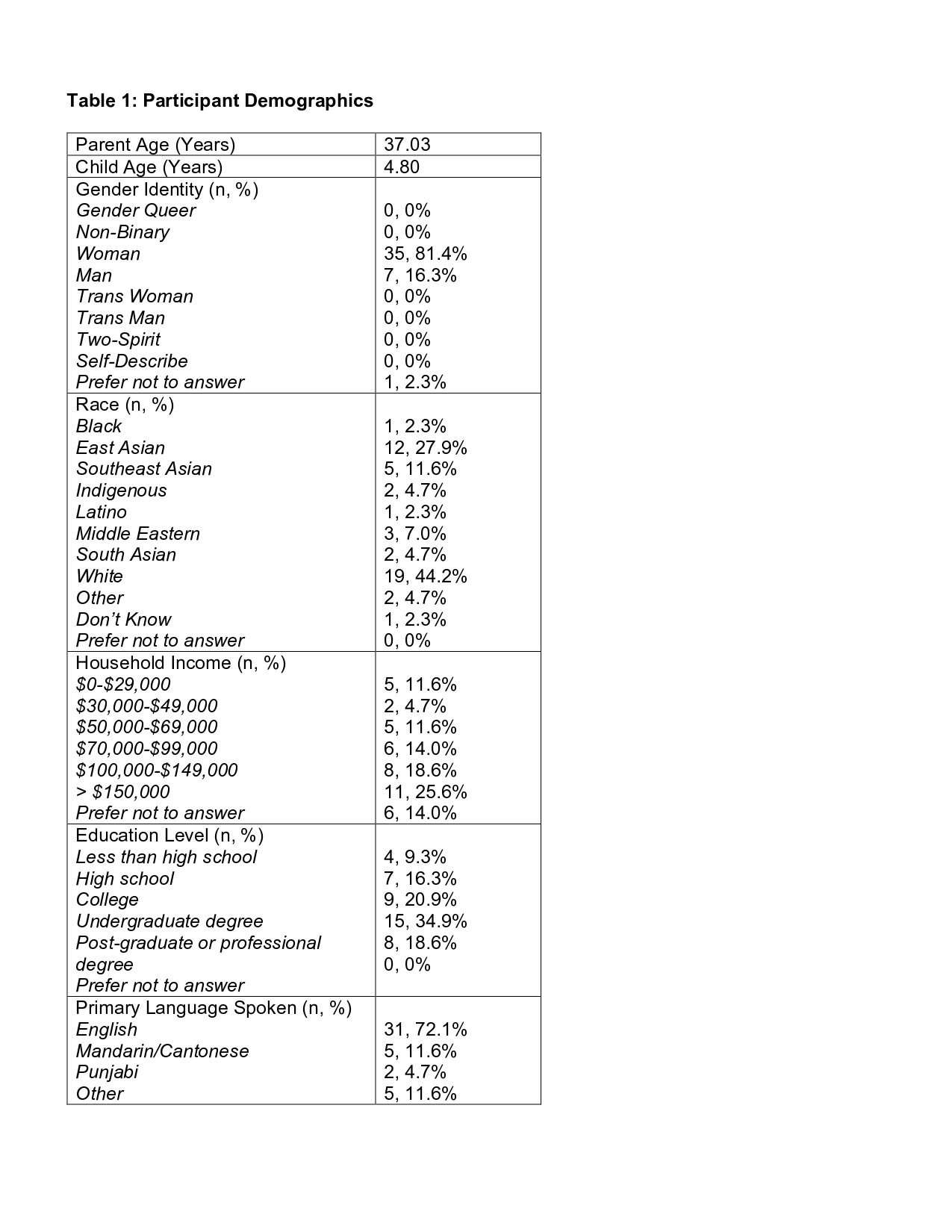
A total of 50 caregivers filled out the cross-sectional survey. Table 1 describes participant demographics. 58% (n=25) of participants were from local communities and 37% (n=16) were from areas > 50 km from our centre. 84% (n=36) of hospital stays were unplanned.
Participants paid an average of $1056 of out-of-pocket costs during their admission. Those from local communities paid an average of $226, while those from away paid an average of $2210 (t(42) = 1.92, p < 0.05). The most significant out-of-pocket costs were attributed to transportation and co-traveller expenses. 56% (n=24) paid out-of-pocket transportation costs, averaging $212 and 79% (n=34) had co-travellers. Of those who had out-of-pocket costs, 20% (n=8) reported difficulty in paying for these costs.
Conclusion(s):
To our knowledge, this study is the first to look at the socioeconomic barriers facing families travelling to a tertiary pediatric hospital in Canada. We found patients from outside the local area had longer length of stay and higher out-of-pocket costs associated with hospitalization, highlighting gaps in resources currently available to support these families.