Developmental and Behavioral Pediatrics: Autism
Developmental and Behavioral Pediatrics 2
565 - Adaptive and Behavioral Profiles of Autistic Youth With & Without Co-Occurring Mental Health & Neurodevelopmental Disorders: A Latent Class Analysis
Publication Number: 565.109
Neelkamal Soares, MD (he/him/his)
Professor, Pediatric & Adolescent Medicine
Western Mich Univ Homer Stryker MD Sch of Medicine
Kalamazoo, Michigan, United States
Presenting Author(s)
Background:
Diagnosis of autism spectrum disorder (ASD) relies on clinical observation and history of behavior to meet specific criteria. Neurodevelopmental and mental health comorbidities can impact diagnostic validity across clinicians. Latent class analysis (LCA) is a helpful statistical procedure for understanding diagnostic subgroups and developmental trajectories among children with heterogeneous manifestations of ASD (Pickles et al, 1995).
Objective: This study uses LCA to optimize subgroup identification based on functional level and associated comorbidities using common psychometric tools {Behavioral Assessment System for Children (BASC-3); Vineland (VABS-3} in a pediatric population at a single autism center.
Design/Methods:
This retrospective study reviewed electronic health record (EHR) data of a single diagnostic center over a 3-year period (2018-2021). Demographic information, clinical assessment results of adaptive, behavior, cognitive, autism evaluation tool results, and ASD diagnosis and other secondary diagnoses for 191 unique patients were extracted. We tested differences between known groups as well as additional latent groups. The “known groups” approach involved contrasting means across the BASC and VABS variables. The exploratory latent class approach tested the presence of latent subgroups guided by the likelihood ratio test, and fit indices such as BIC, CAIC, cmP(k) and AICc. Entropy estimates were given consideration but did not contribute to the latent class enumeration process.
Results:
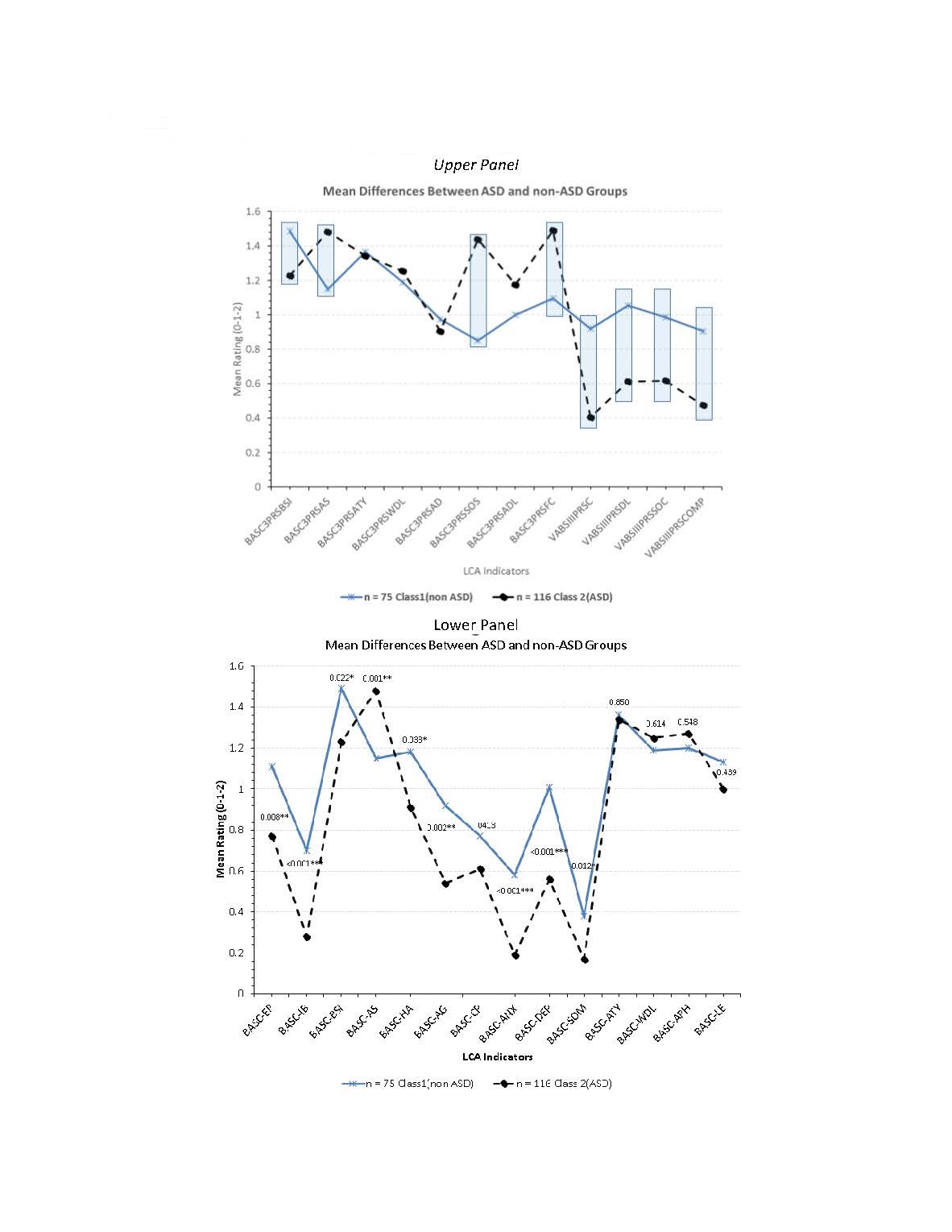
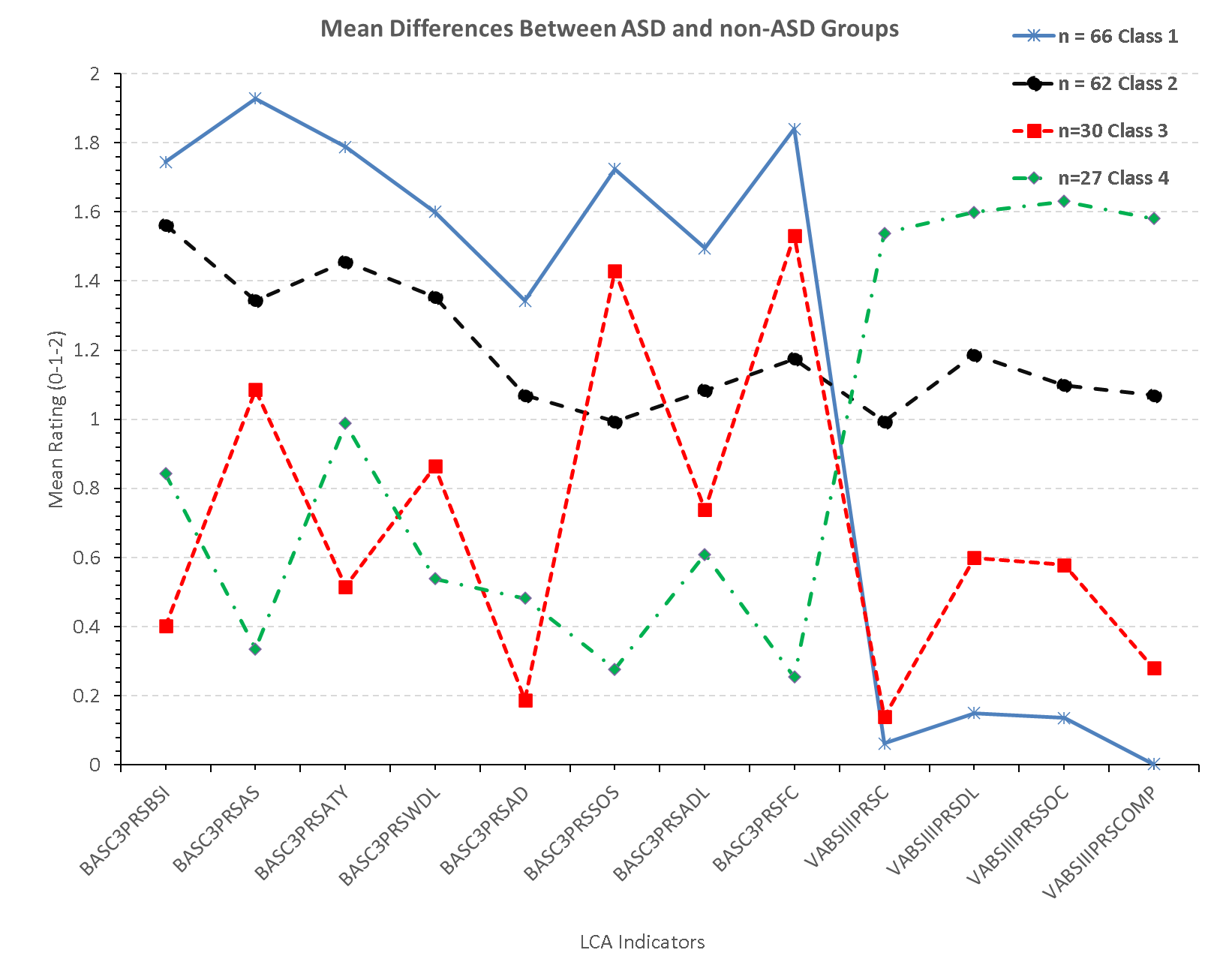
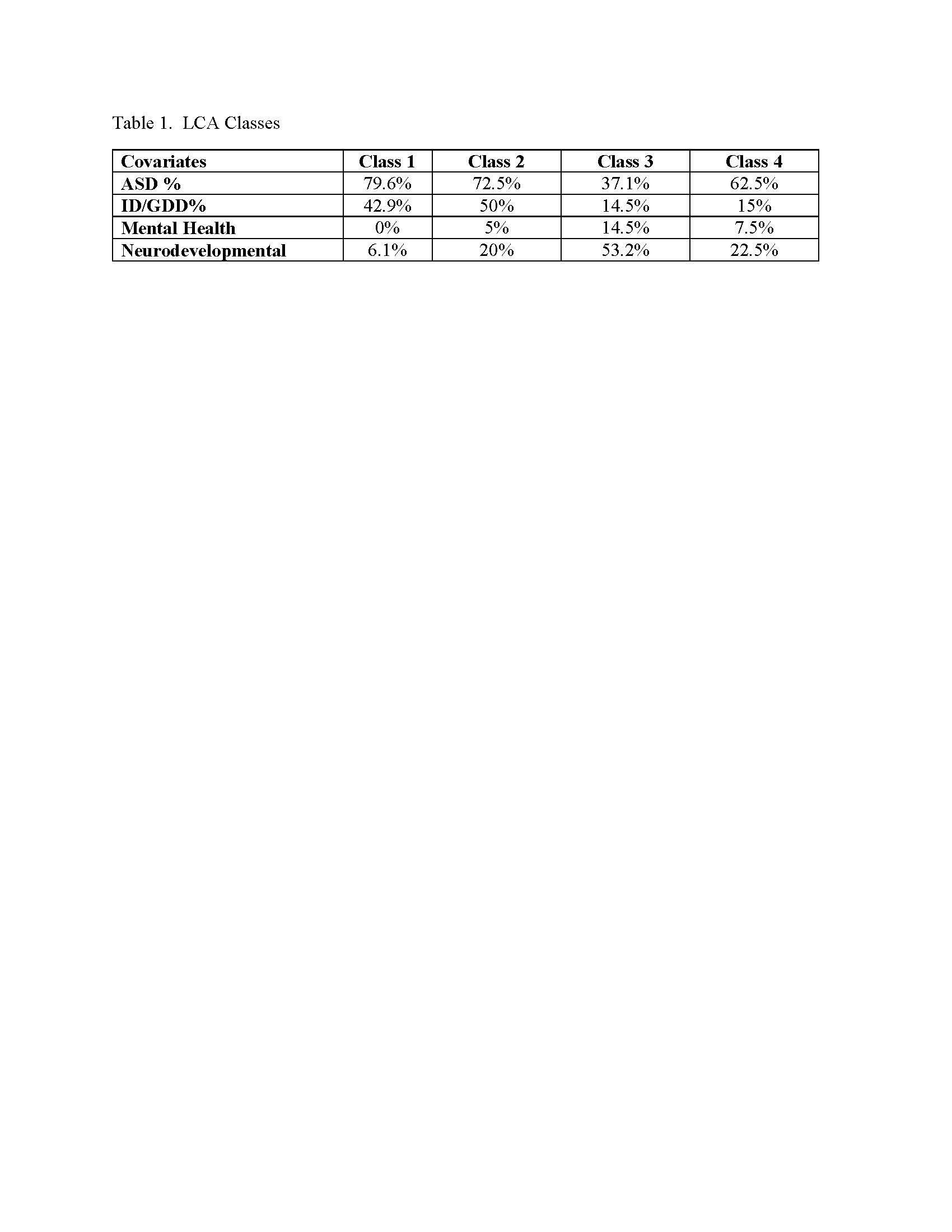
There were significant between-groups (ASD vs. non-ASD) differences on several subscales (Figure 1, upper panel). Lower panel displays significant differences on BASC emotional/behavioral variables. Figure 2 displays exploratory LCA with emergence of 4 distinct latent subgroups supported by fit indices and Loglikelihood difference test. Classes 1 and 2, respectively the youngest and oldest classes (see Table 1), were predominantly ASD classes, with class 2 exhibiting more co-occurring conditions. Class 3 was a lower incidence ASD class with higher prevalence for mental health and neurodevelopmental disorders. Lastly, class 4 had a lower incidence of ASD, higher adaptive skills relative to the other classes, but more neurodevelopmental disorders.
Conclusion(s):
LCA of common adaptive and behavioral measures can distinguish between sub-groups of pediatric patients referred for ASD evaluations and can assist in a more targeted triage of cases based on severity. Older patients are likely to have more comorbidities, with adaptive scores differentiating those with greater or lesser behavioral health needs.