Health Equity/Social Determinants of Health
Health Equity/Social Determinants of Health 2
528 - Current Practices for Engaging Families with Limited English Proficiency in the NICU
Friday, April 28, 2023
5:15 PM - 7:15 PM ET
Poster Number: 528
Publication Number: 528.117
Publication Number: 528.117
Zayna M. Bakizada, Doernbecher Children's Hospital at Oregon Health & Science University, Portland, OR, United States; Jessica Hoffman, Doernbecher Children's Hospital at Oregon Health & Science University, Portland, OR, United States; Astrid S. Platteau, Oregon Health & Science University School of Medicine, tualatin, OR, United States; Anita Khut, Oregon Health & Science University, Sherwood, OR, United States; Devlynne S. Ondusko, Oregon Health & Science University School of Medicine, Portland, OR, United States

Zayna M. Bakizada, MD (she/her/hers)
Resident Physician
Doernbecher Children's Hospital at Oregon Health & Science University
Portland, Oregon, United States
Presenting Author(s)
Background: Compared to English-speaking mothers, non-English-speaking mothers’ infants have worse outcomes in the Neonatal Intensive Care Unit (NICU), which after adjusting, seems to be most likely related to communication practices. For example, bedside nurses must communicate with each family multiple times a day in order to engage them in infant cares (e.g., feeding time, diaper changes, bathing).
Objective: The objective was to assess nursing perspectives on family-nursing language discordance and evaluate the process of inviting families with limited English proficiency (LEP) to participate in infant cares in the NICU.
Design/Methods: A web-based ten-question survey was administered to nurses working at a level IV regional referral NICU. The survey evaluated current communication practices in the setting of language discordance and nursing satisfaction with these practices.
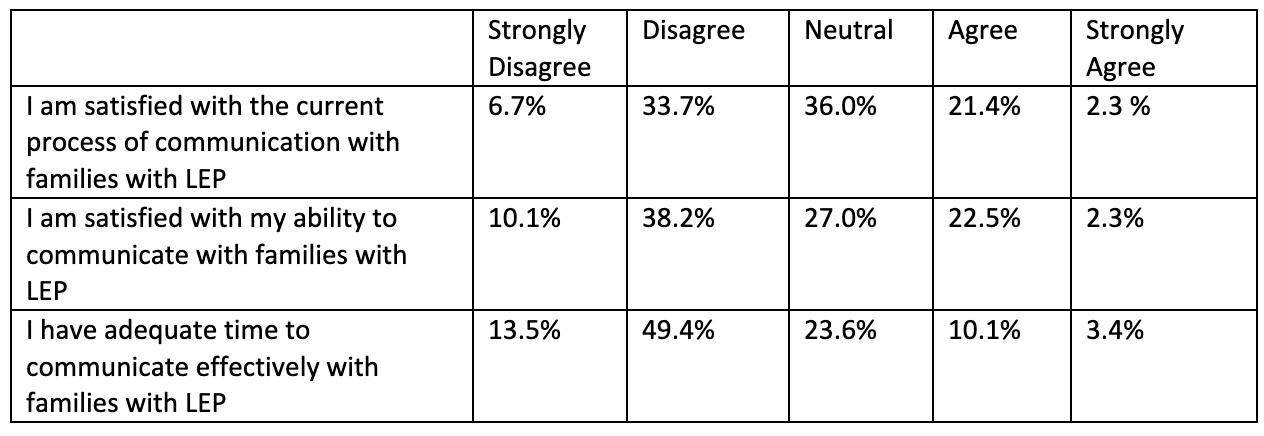
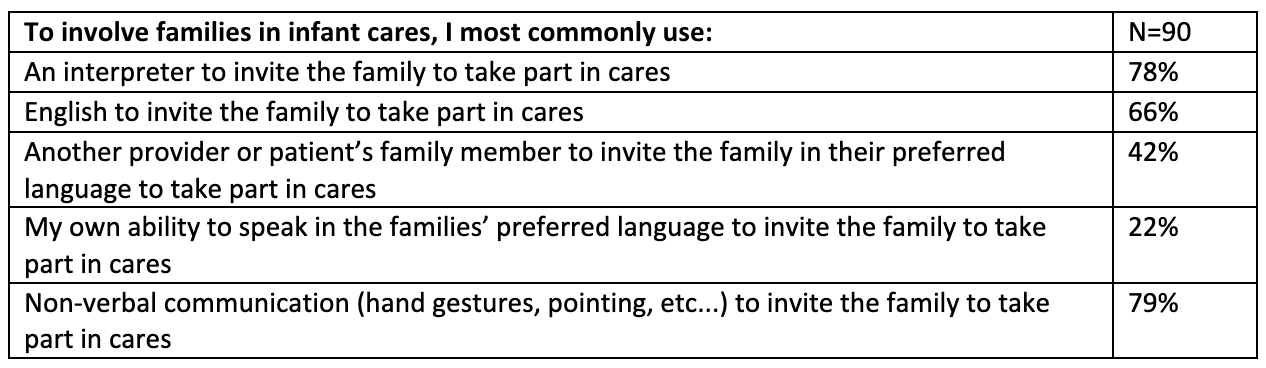
Results: Ninety nurses completed the survey, a 64% response rate. Of the nurses surveyed, most (58%) did not speak any Spanish. Of the 5.6% (n=5) that reported speaking Spanish at the level of Good to Advanced (as defined by the Association of American Medical Colleges), only one respondent endorsed passing the bilingual provider certification exam required by the institution. Less than a quarter of the respondents (24%) endorsed satisfaction with the current process of communication with families with LEP [Table 1]. More than half (63%) of the nurses disagree that they have enough time to communicate effectively with families with LEP. While use of a certified interpreter is a practice standard in the setting of language discordance, only 78% of respondents endorsed using an interpreter to invite a family with LEP to take part in bedside cares for their baby. A similar number of respondents (79%) endorsed using non-verbal communication (hand gestures, pointing, etc.) to invite the family to take part in cares [Table 2].
Conclusion(s): In this single center study we found that current practices of inviting families with LEP to participate in infant cares are inadequate. The current practices may negatively impact family involvement, a known contributor to infant outcomes in the NICU. The next step of this study is the implementation of a language card, which will be used as a bedside communication assistance tool for family involvement in infant cares, in hopes of both improving nursing satisfaction and reducing inequities.