Hospital Medicine: Hospital Medicine Quality Improvement
Hospital Medicine 1
746 - Feed The Baby! A Quality Improvement Intervention to Increase Enteral Feeding in Bronchiolitis
Publication Number: 746.119

Rebecca A. Veele, MD (she/her/hers)
Resident
Michigan State University College of Human Medicine
Grand Rapids, Michigan, United States
Presenting Author(s)
Background:
Recent studies identify enteral feeding as a safe alternative to intravenous fluid hydration for inpatients with bronchiolitis receiving respiratory support. Studies show enteral nutrition can improve vital signs, shorten time on hi-flow nasal cannula (HFNC), and is associated with reduced length of stay (LOS).
Objective:
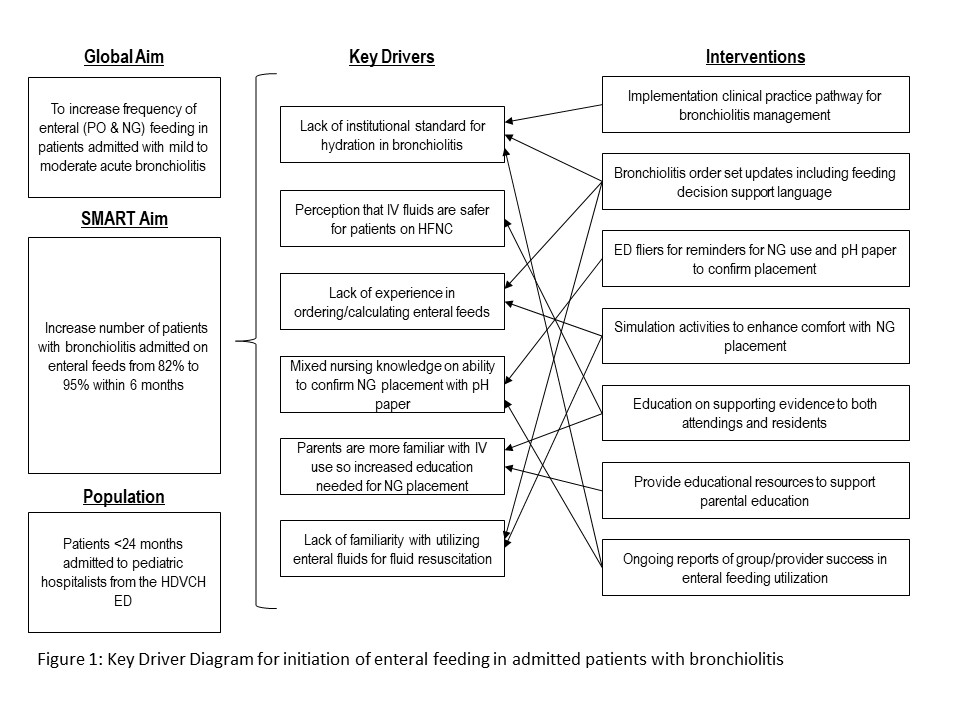
Within 6 months, increase initiation of enteral feeding (via oral or nasogastric routes) from 82% to 95% of patients with mild to moderate bronchiolitis, including on HFNC, at the time of admission.
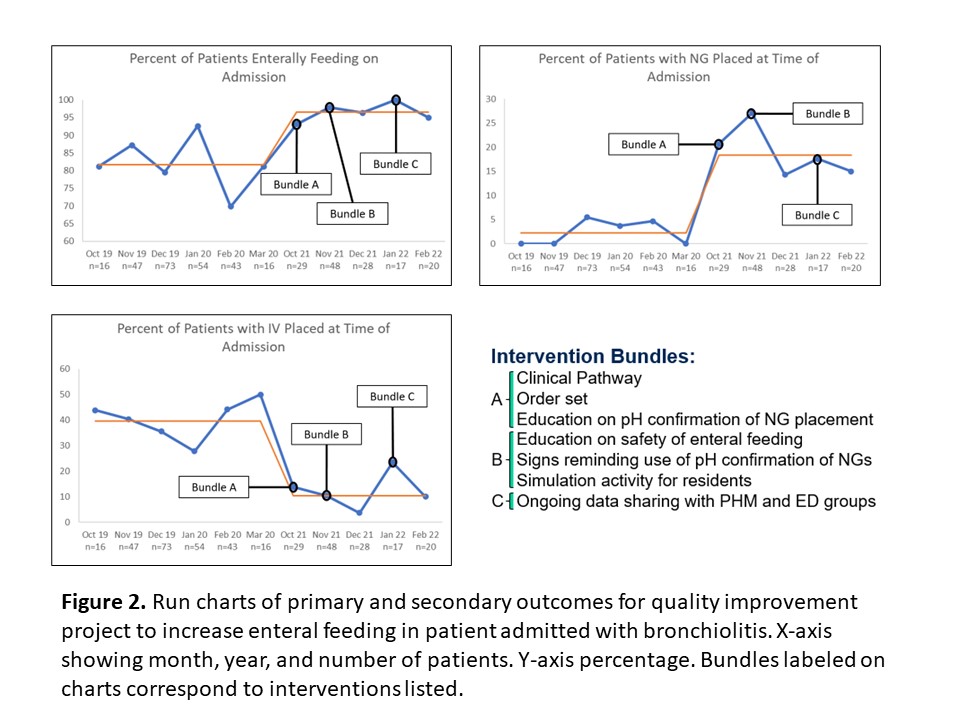
Design/Methods: A multidisciplinary team at our tertiary children’s hospital used quality improvement methodology to develop and test interventions targeted at increasing the use of enteral feeding in patients admitted with bronchiolitis. Patients with severe bronchiolitis or admitted to the ICU were excluded. Interventions included development and implementation of a Bronchiolitis Clinical Practice Pathway with an embedded guideline and order set to support enteral feeding. Following implementation, educational sessions were provided to our Pediatric Emergency Medicine faculty, Pediatric Hospital Medicine Faculty, and Residents and Fellows in both specialties. A simulation session was held with Pediatric Residents. Retrospective chart review was conducted. Run charts and statistical process control charts were used to track adoption of enteral feeding over time. Results were shared with PEM and PHM groups monthly.
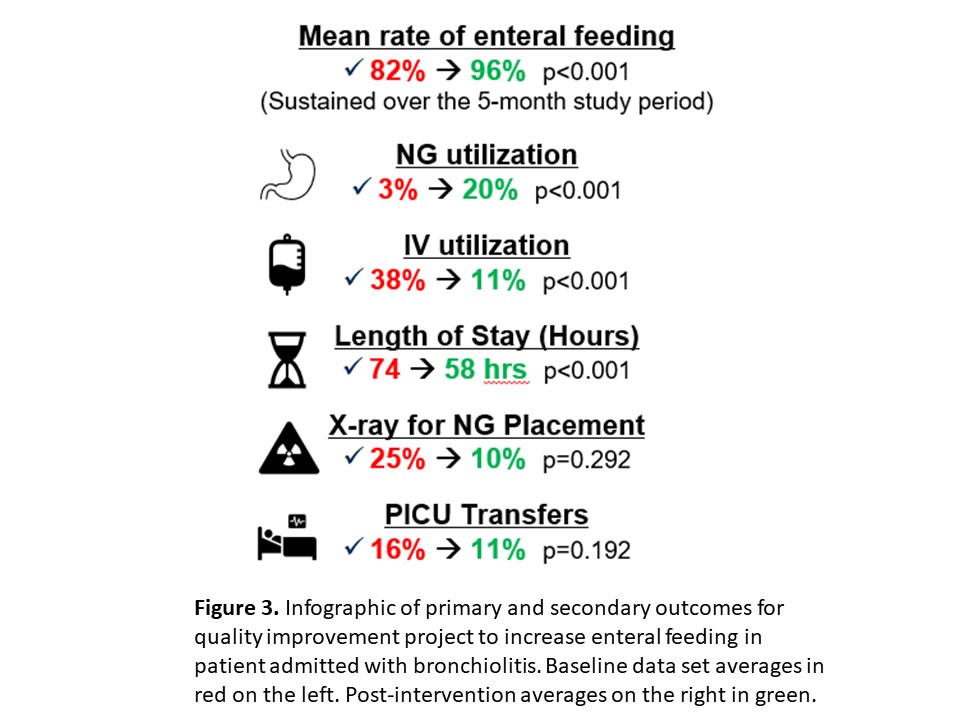
Results: Median rate of initiation of enteral feeding increased from 82% of bronchiolitis patients pre-intervention to 96% of patients post-intervention with a shift in month-to-month rates. Mean rate of IV placement decreased from 38% to 11%. Mean rate of NG placement rose from 3% to 20%. A post-intervention shift was seen with both IV and NG placement rates. No increase in ICU transfers was found (16% baseline, 11% post-intervention), and total hospital LOS decreased from 74 hours at baseline to 58 hours post-intervention.
Conclusion(s):
Implementation of a Bronchiolitis Clinical Practice Pathway including an embedded guideline and order set to support enteral feeding were effective at increasing initiation of enteral feeding in patients with mild to moderate bronchiolitis admitted to the hospital. A formalized education bundle including simulation activities effectively supported these efforts. This statistically significant increase resulted in decreased LOS without an increase in ICU transfers.