Children with Chronic Conditions
Children with Chronic Conditions 3
83 - Mental and Behavioral Health Access and Needs Among Children with Medical Complexity
Sunday, April 30, 2023
3:30 PM - 6:00 PM ET
Poster Number: 83
Publication Number: 83.305
Publication Number: 83.305
Kristina Malik, Children's Hospital Colorado, Aurora, CO, United States; Jonah Stoller, University of Colorado School of Medicine, Denver, CO, United States; Verenea Serrano, University of Colorado School of Medicine, Denver, CO, United States; Charlene Shelton, ACCORDS, University of Colorado Denver, Aurora, CO, United States; Christopher J. Stille, University of Colorado School of Medicine, Aurora, CO, United States; Lisa Maynes, Family Voices National, Colchester, VT, United States; Roxana Delgado-Martinez, University of California, Los Angeles David Geffen School of Medicine, Los Angeles, CA, United States; Dinorah Zanger, UT Health Science Centers, Houston, TX, United States; Diana J. Martinez Castillo, University of Texas-Houston, Houston, TX, United States; Carlos Lerner, Dept Pediatrics UCLA, Los Angeles, CA, United States; Ricardo A. Mosquera, University Of Texas Houston, Houston, TX, United States

Kristina Malik, MD (she/her/hers)
Assistant Professor
Children's Hospital Colorado/University of Colorado
Aurora, Colorado, United States
Presenting Author(s)
Background: Children with medical complexity (CMC) have increased unmet mental and behavioral health (MBH) needs when compared to non-complex peers. National survey data shows the unmet need is due to medical complexity itself (not confounded by race, income, or insurance). Further research of why this gap exists has not been published. Clinically, this is thought due to multiple factors including the unique MBH needs seen in CMC and their families. In general, CMC are at increased risk for health disparities such as health care access. Caregiver reports might provide clues that would be critical in developing best practices for MBH for CMC and their families.
Objective: To determine the behavioral and mental health needs of CMC and their families and how well those needs are met through existing services.
Design/Methods: A multi-site, multidisciplinary team including caregivers of CMC developed an interview guide using a phenomenology approach. Participants were recruited from three academically affiliated complex care programs. Semi-structured interviews with 30 caregivers of CMC (5 English-speaking and 5 Spanish-speaking at each site) were conducted. Interviews were audio recorded and professionally transcribed. Independent coding was performed by members of the study team, followed by transcript review and discussion of initial themes until thematic saturation was reached. Dedoose software was used for data organization and retrieval.
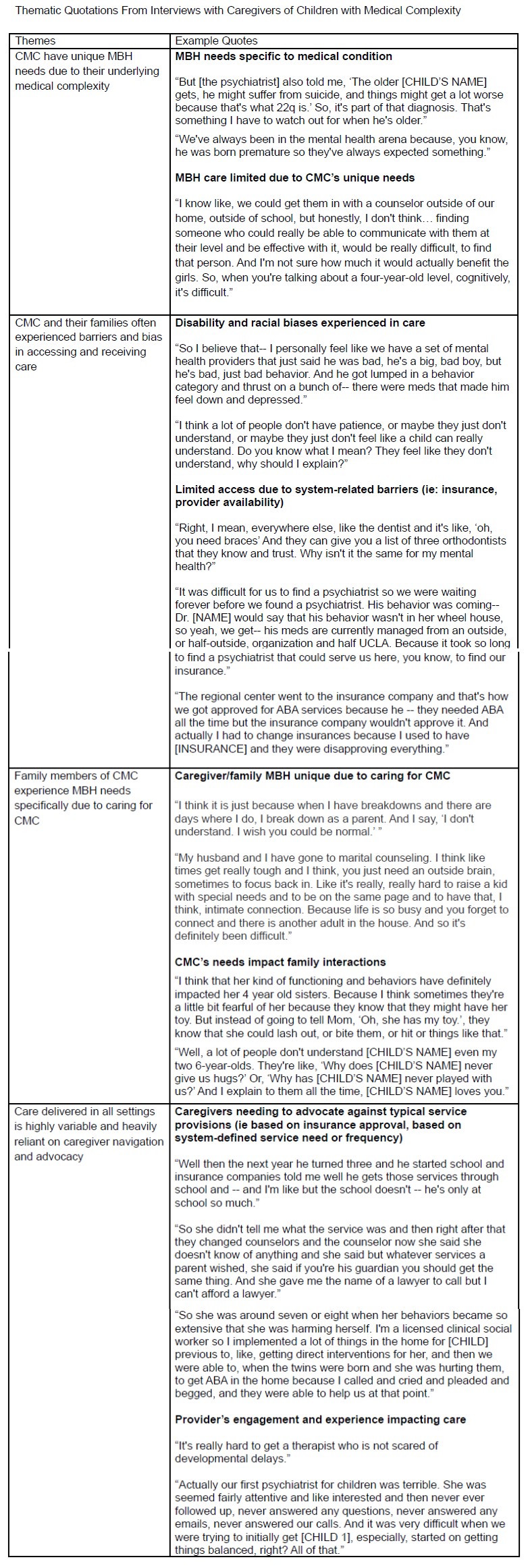
Results: Four key themes emerged: 1) CMC have unique MBH needs due to their underlying medical complexity; 2) CMC and their families often experienced barriers and bias in accessing and receiving care; 3) family members of CMC experience MBH needs specifically due to caring for CMC; and 4) care delivered in all settings is highly variable and heavily reliant on caregiver navigation and advocacy. In addition, caregivers reported integrated MBH for CMC was rare but highly valued.
Conclusion(s): CMC and their families may experience unique MBH needs and access barriers related to the child’s medical complexity. Care delivered through MBH integrated into complex care medical homes may help mitigate variability and reduce barriers. Unmet needs create vulnerabilities in both the medical and MBH spheres (ie: polypharmacy, care coordination) that require tailored supports and interventions for this population.