Neonatal Hematology & Bilirubin Metabolism
Neonatal Hematology & Bilirubin Metabolism 2: Hematology
129 - Circulating Extracellular Vesicles During Perinatal Adaption; Unique Patterns In Very Preterm Infants
Publication Number: 129.239

Claire A. Murphy, MB, PhD
Specialist Registrar Neonatology
Rotunda Hospital
Dublin, Dublin, Ireland
Presenting Author(s)
Background:
Extracellular vesicles (EVs), membrane-enclosed nanoparticles released from cells, have been investigated in neonatal haemostasis, as biomarkers of preterm pathologies and therapeutic drug targets. However, little is known about the circulating EVs during perinatal adaption.
Objective:
To describe circulating EVs in preterm infants during the first two weeks of life, comparing them to healthy full-term infants.
Design/Methods:
The EVENT Study was a prospective observational study at a single tertiary NICU. Ethical approval was obtained and parental consent was required for participation. Blood samples were collected in sodium citrate from the umbilical cord, and postnatal samples on day 1, day 3 and two weeks. Platelet-poor plasma (PPP) was prepared (3000 RPM x 6 minutes x 2). Small EVs (SEVs) (< 200nm) were assessed by nanoparticle tracking analysis in PPP. Large EVs (LEVs) were evaluated by flow cytometry (FACS Canto II) following isolation at 20,800 xg and staining of surface antigens. The procoagulant activity of Tissue factor EVs (TF-EV) was measured by the ZYMUPHEN MP Activity kit.
Results:
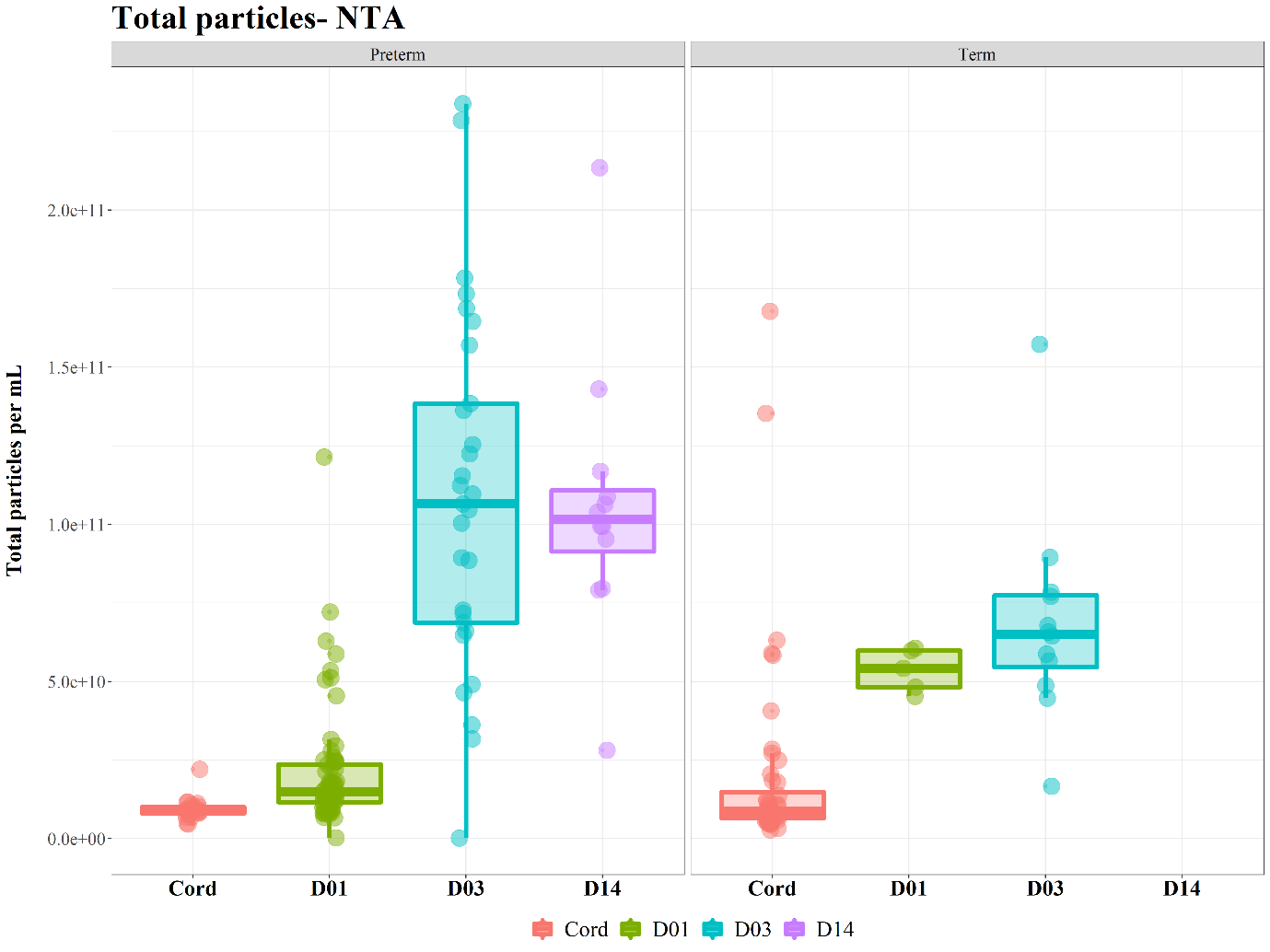
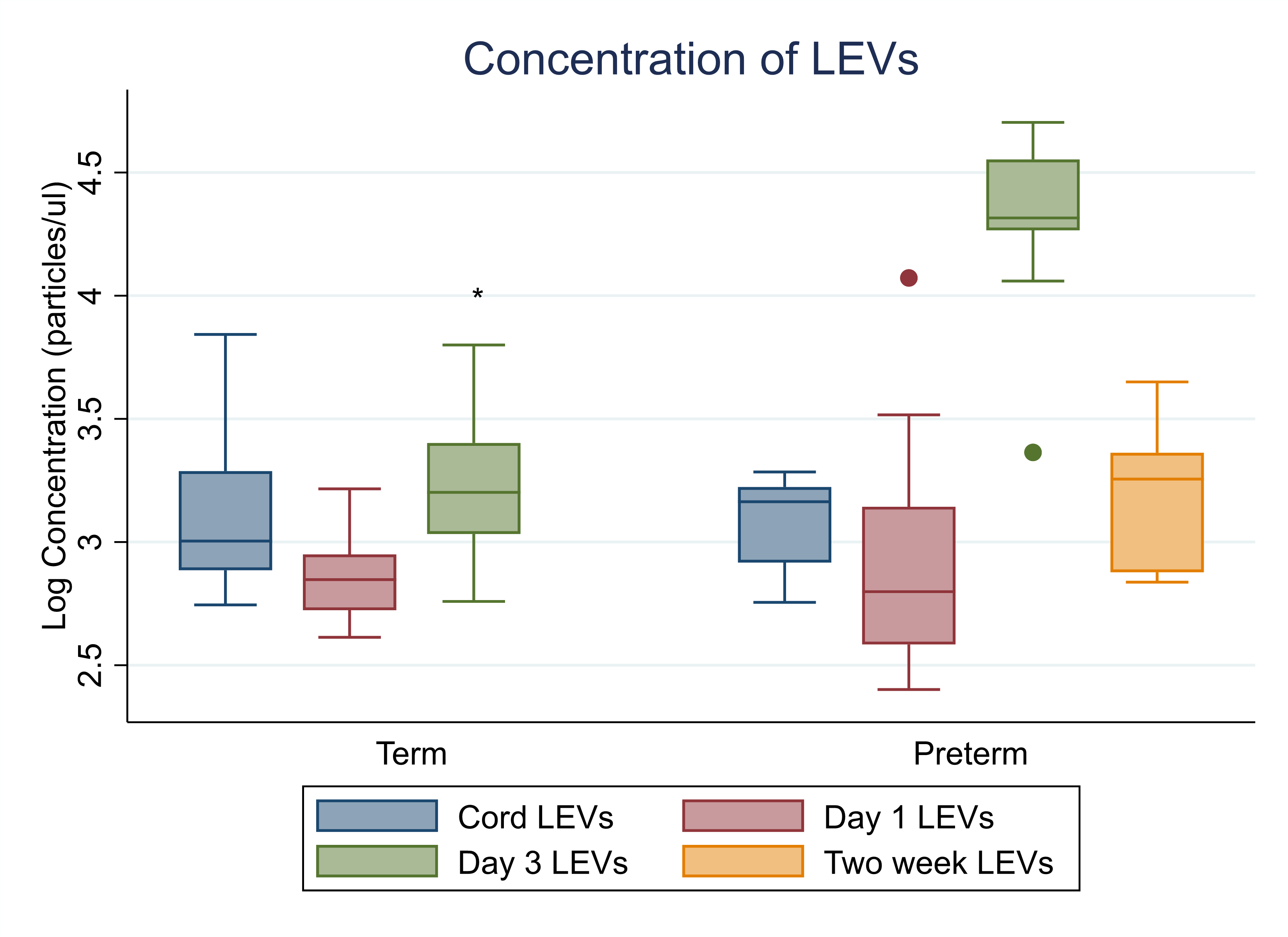
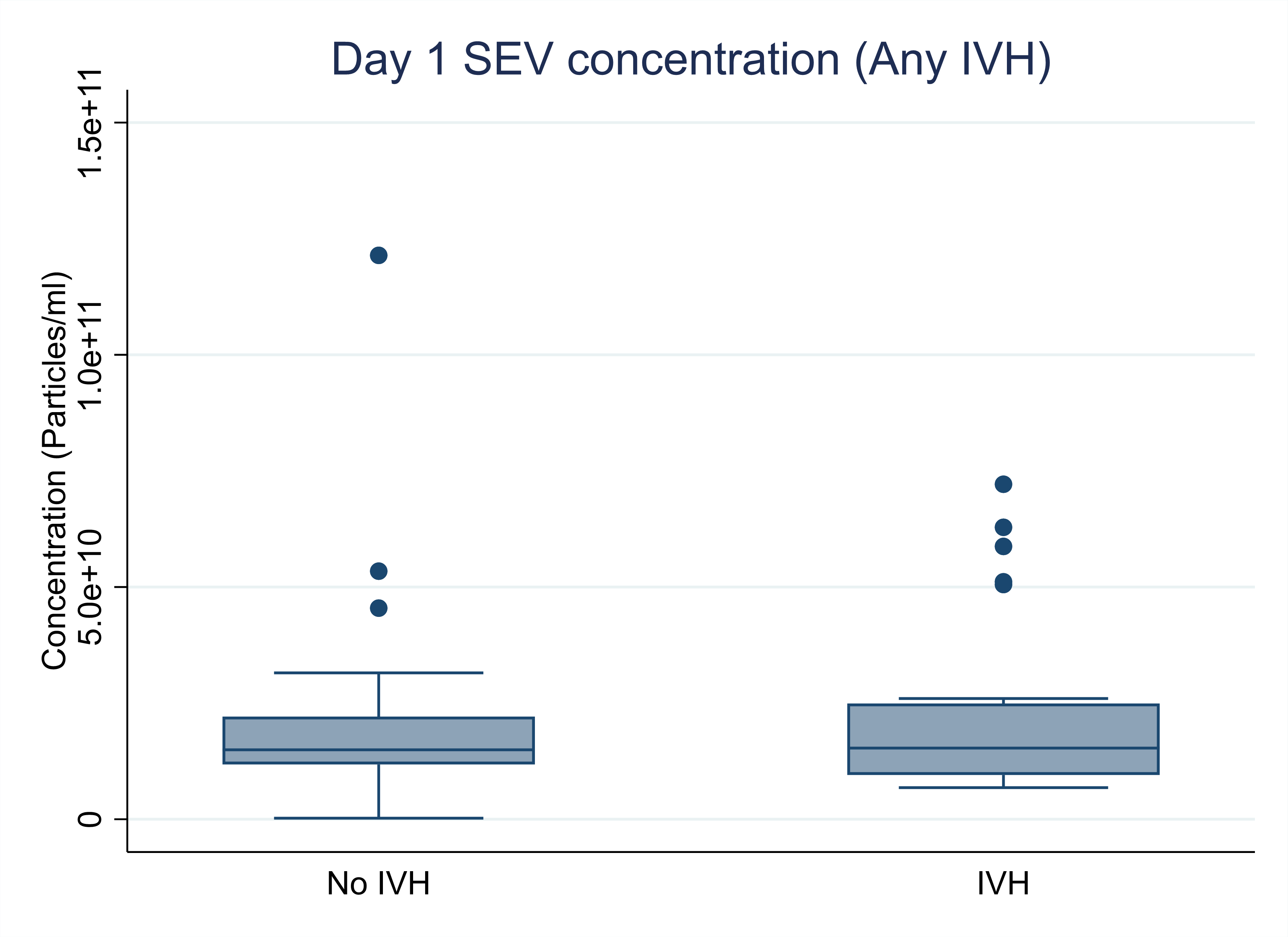
101 preterm infants were recruited (median gestation 28.3 weeks & birth weight 1.1kg) and 66 full-term controls. The concentration and origin of SEVs and LEVs were similar in preterm and term infants in cord blood samples. However, the SEV (Figure 1) and LEV (Figure 2) concentrations increased significantly between Day 1 and Day 3 of life in preterm infants, and were both significantly higher than term infants on Day 3 (adjusted p=0.02 and p< 0.01 respectively). On Day 3, the concentration of platelet (CD42b & CD62P), endothelial (VEGFR2) and tissue factor LEVs were significantly higher in the preterm group. Annexin V +, CD 41 (platelet) and white cell (CD45) LEVs were similar in preterm and term infants at each timepoint studied. The procoagulant TF-EV concentration was similar between preterm and term infants in both cord (p=0.16) and postnatal samples (p= 0.25). The EV content of cord and postnatal samples on Day 1 of life were different. The concentration of SEVs did not differ between infants who subsequently developed an intraventricular haemorrhage and those that did not (p=0.88) (Figure 3).
Conclusion(s):
This is the first study to characterise circulating EVs during perinatal adaption, with a unique EV profile seen in preterm infants on Day 3 of life. Future studies must explore whether these changes represent the initiation of inflammatory pathologies or maladaptation to extra-uterine life in preterm infants.