Neonatal-Perinatal Health Care Delivery: Epidemiology/Health Services Research
Neonatal-Perinatal Health Care Delivery 4: Epi/HSR Utilization, Cost, Outcomes
779 - Hospital and medication utilization following discharge from the NICU for extreme premature infants enrolled in the PENUT Trial
Publication Number: 779.248

Sarah E. Kolnik, MB MBA (she/her/hers)
Assitant Professor of Pediatrics
University of Washington - Seattle Children's Hospital
Seattle, Washington, United States
Presenting Author(s)
Background:
Infants born preterm are well-documented to require more extensive healthcare resources and follow-up than infants born term. However, small studies looking at long-term utilization suggest that not all follow-up differences can be attributed to prematurity comorbidities, limiting our understanding of long-term healthcare utilization among formerly preterm children.
Objective: The aim of this descriptive analysis was to better understand hospital and medication utilization after discharge in infants born extremely preterm (EP) at 30-60 months corrected age (CA), and to compare the rate of emergency room (ER)/urgent care visits and hospitalizations to the general population.
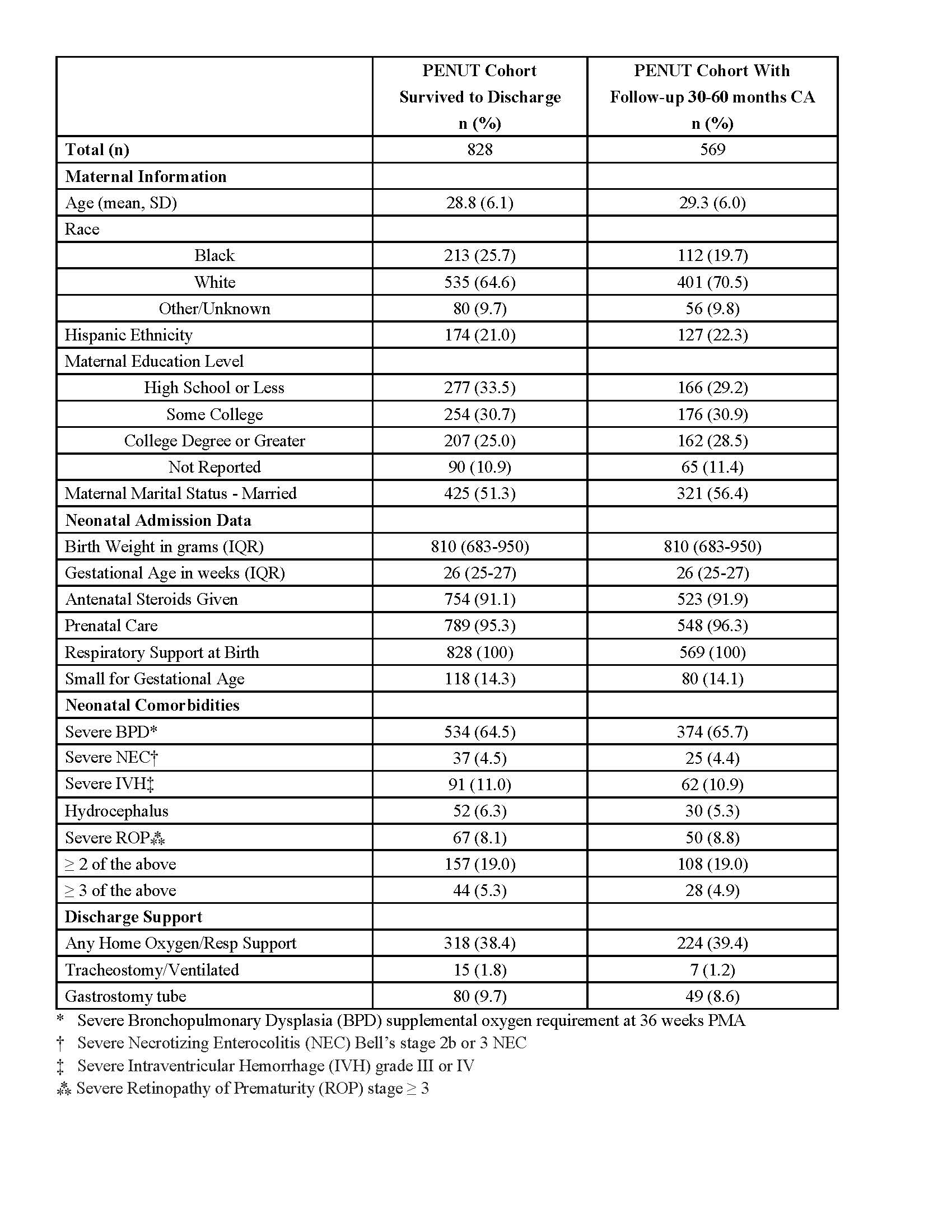
Design/Methods: This is a post hoc analysis of EP infants born between 24 0/7 and 27 6/7 weeks’ gestation enrolled in the Preterm Erythropoietin Neuroprotection Trial (PENUT). Infants with at least one phone questionnaire follow-up between 30 and 60 months CA were included. In addition to maternal, neonatal, and neonatal intensive care unit stay information provided by the PENUT database, questionnaire clinical information collected included ER/urgent care visits, hospitalizations, and medication use. Comparison general population data was collected from National Center for Health Statistics National Health and Nutrition Examination Survey (NHANES) and Agency for Healthcare Quality and Research (AHQR) via the Healthcare Cost and Utilization Project (HCUP) database.
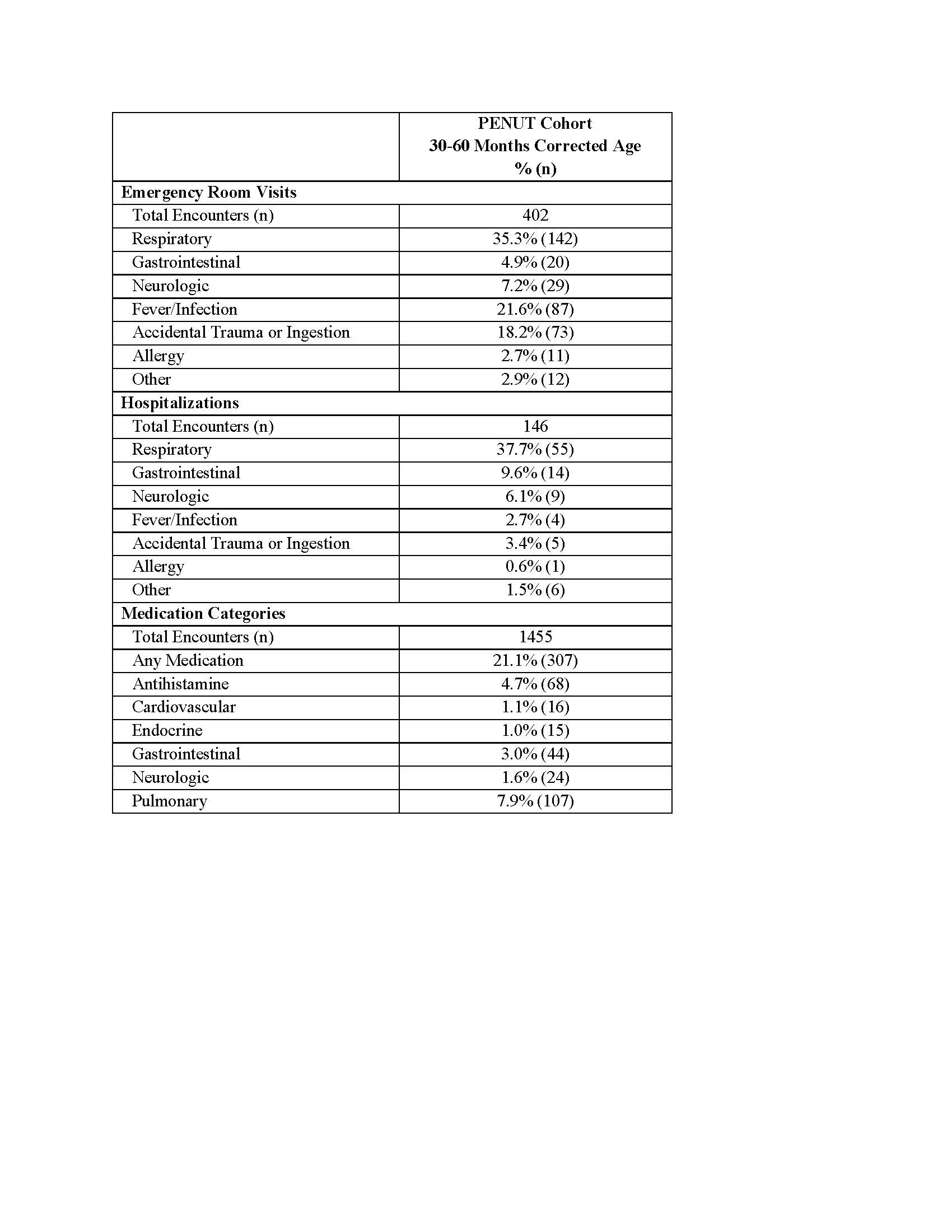
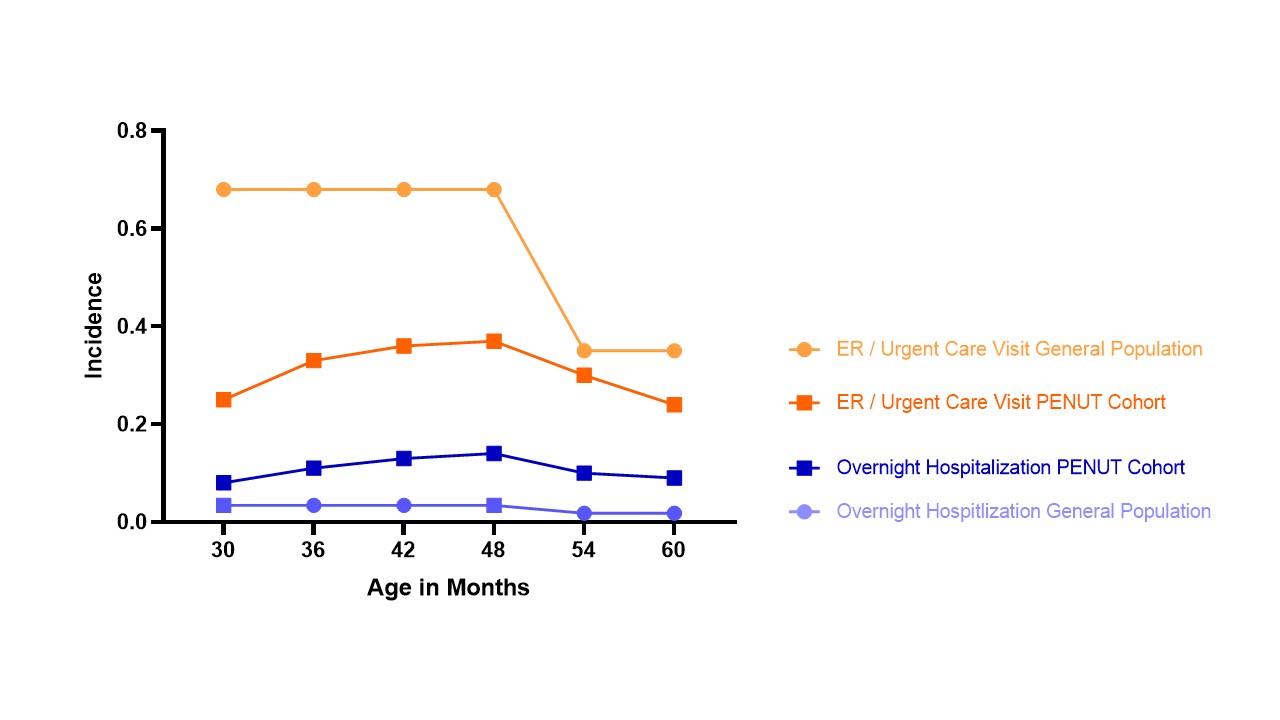
Results: Among the n=569 EP infants included in this analysis, maternal, infant, and NICU data for those who survived to discharge and for those with follow-up data available are similar except that infants followed were less likely to have a mother that identified as black (p< 0.0001) (Table 1). The total number of ER/urgent care visits and hospitalizations by cause as well as reports of medication usage by type are summarized in Table 2. The most common reason for ER/urgent care visits, hospitalizations, and medication usage was for respiratory issues. Compared to the general population, EP infants had less ER/urgent care visits, but more hospitalizations.
Conclusion(s): The lower rate of ER/urgent care utilization by EP infants may be indicative of greater access to alternative healthcare resources, while the greater incidence of hospitalizations may be secondary to a higher baseline severity of illness or need for procedures. Further analysis comparing details of care are needed to direct future efforts to improve healthcare and medication utilization by EP infants following NICU discharge.