Emergency Medicine: All Areas
Emergency Medicine 7
370 - Implementation of Predictive Decision Support for Pediatric Septic Shock: A Qualitative Study of Emergency Clinicians’ Experience
Publication Number: 370.211

Halden F. Scott, MD, MSCS (she/her/hers)
Associate Professor of Pediatrics
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background: Timely treatment of pediatric septic shock has improved, but diagnosis remains challenging. Surviving Sepsis guidelines highlight that screening tools for pediatric sepsis are an important knowledge gap/research need. Clinical decision support (CDS) in the Electronic Health Record (EHR) may improve diagnosis; however prospective trials of CDS have not demonstrated improved outcomes.
Objective: To assess providers’ attitudes about CDS designed to predict septic shock in the Emergency Department (ED), to understand implementation barriers, facilitators and outcomes.
Design/Methods: This qualitative study was part of a prospective, stepped-wedge trial of novel CDS in 4 pediatric EDs. The CDS was built on published, validated machine learning models that used vital signs, labs, patient factors to predict septic shock. CDS was implemented as an Epic Best Practice Alert (BPA), designed with provider testing and feedback (Fig 1). We identified and purposively sampled providers who saw the BPA in their ED practice. Consenting providers participated in semi-structured interviews with a qualitative analyst. Interviews were recorded and professionally transcribed. The interview guide and coding domains were developed deductively using PRISM, an implementation framework. Transcripts were iteratively reviewed to refine domains and achieve reconciliation; 20% were double-coded. Coded data were analyzed using matrix analysis to identify themes.
Results:
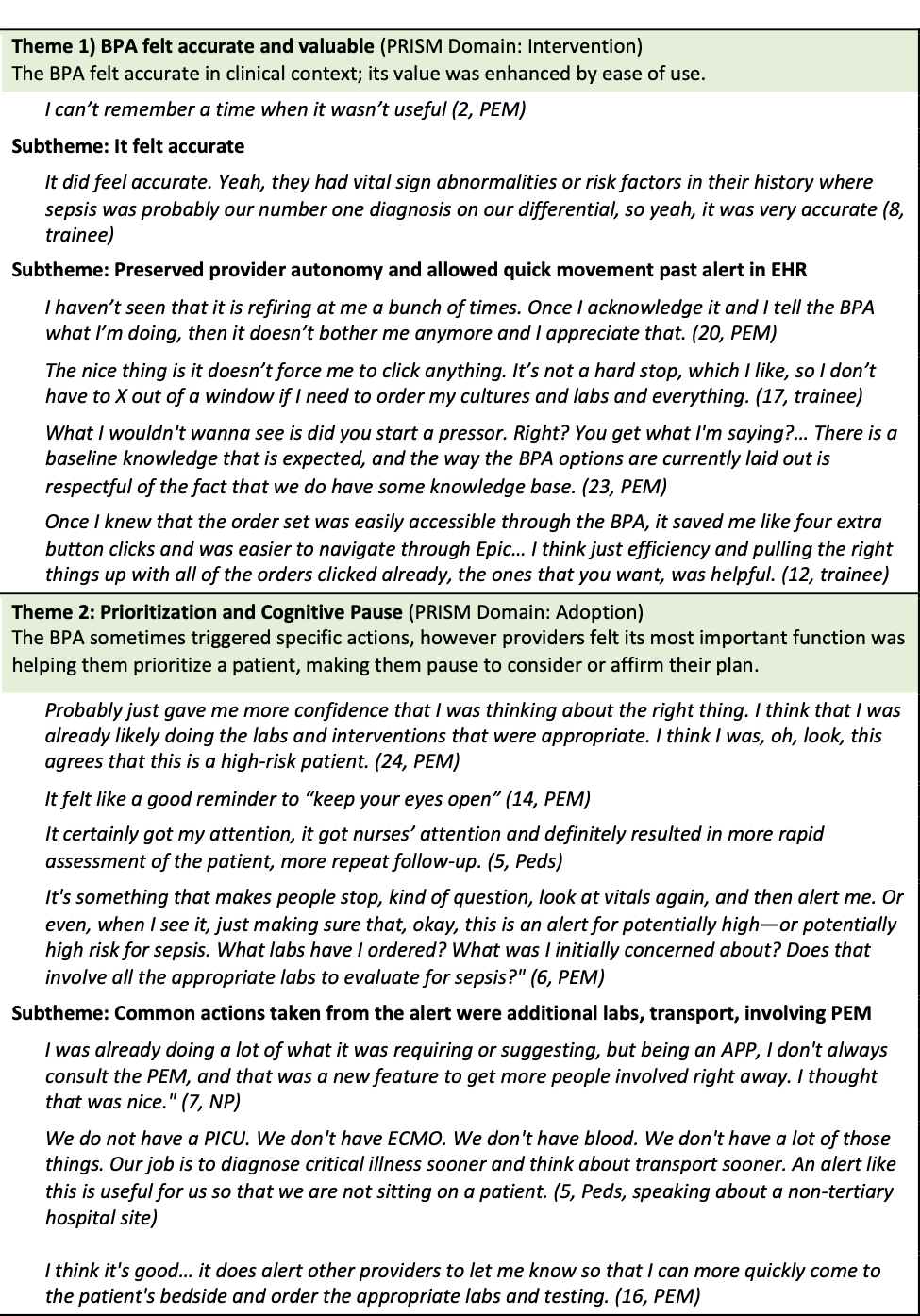
27 ED providers were interviewed; 14 (54%) pediatric emergency physicians, 2 (8%) pediatricians, 3 (12%) advanced practice providers, 7 (27%) trainees. Themes emerged that reflected the function, value, and setting of the BPA [Table 1, 2]:
1) BPA felt accurate and valuable in clinical context
2) Prioritization and cognitive pause (The most important function of the BPA was prioritizing a patient, making providers pause to consider or affirm their plan)
3) Alert fatigue in the physical and electronic ED environment (Interruptions were frequent; BPA didn’t cause fatigue because it felt important)
4) Interaction with sepsis systems (BPA works within sepsis structures, may not improve care on its own)
Conclusion(s): Participants identified that the predictive septic shock BPA was useful in prioritization, and appreciated its low triggering frequency and ease of dismissing. A main benefit of the BPA was risk-stratifying in a busy ED with multiple competing demands. Alert fatigue in the ED and EHR presented a simultaneous challenge and need for this BPA. Participants felt that well-designed decision support could mitigate some, but not all, challenges to ED sepsis care.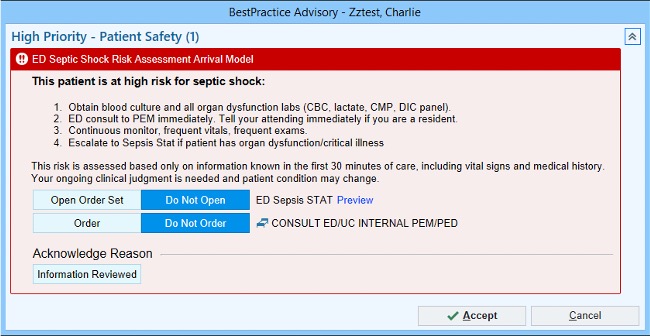
.jpg)
