Nephrology: Clinical
Nephrology 3: Dialysis and Diversity and Equity in Kidney Health
288 - Therapeutic Plasma Exchange for Mechanical Red Cell Hemolysis: A Case Series
Publication Number: 288.252

Chloe E. Douglas, MD (she/her/hers)
PGY-5 Pediatric Nephrology Fellow
University of Washington/Seattle Children's Hospital
Seattle, Washington, United States
Presenting Author(s)
Background: Mechanical red cell hemolysis and elevated serum plasma free hemoglobin (PFH) levels may be seen in pediatric patients requiring mechanical circulatory support devices. Heme pigments released from degradation of hemoglobin in the kidneys may cause acute kidney injury (AKI) via tubular obstruction and direct proximal tubule epithelial cell injury. Therapeutic plasma exchange (TPE) has been utilized to reduce PFH to improve associated morbidity. However, there are limited data and mechanical red cell hemolysis is not included in the current apheresis guidelines.
Objective: To describe the clinical course of three children who received TPE for elevated PFH secondary to mechanical red cell hemolysis.
Design/Methods: Observational report of three patients who received TPE for elevated PFH secondary to mechanical red cell hemolysis at Seattle Children’s Hospital in 2020-2021. Details of patient clinical characteristics, mechanical circulatory support, and TPE prescription were collected. PFH levels were reviewed before and after TPE initiation.
Results:
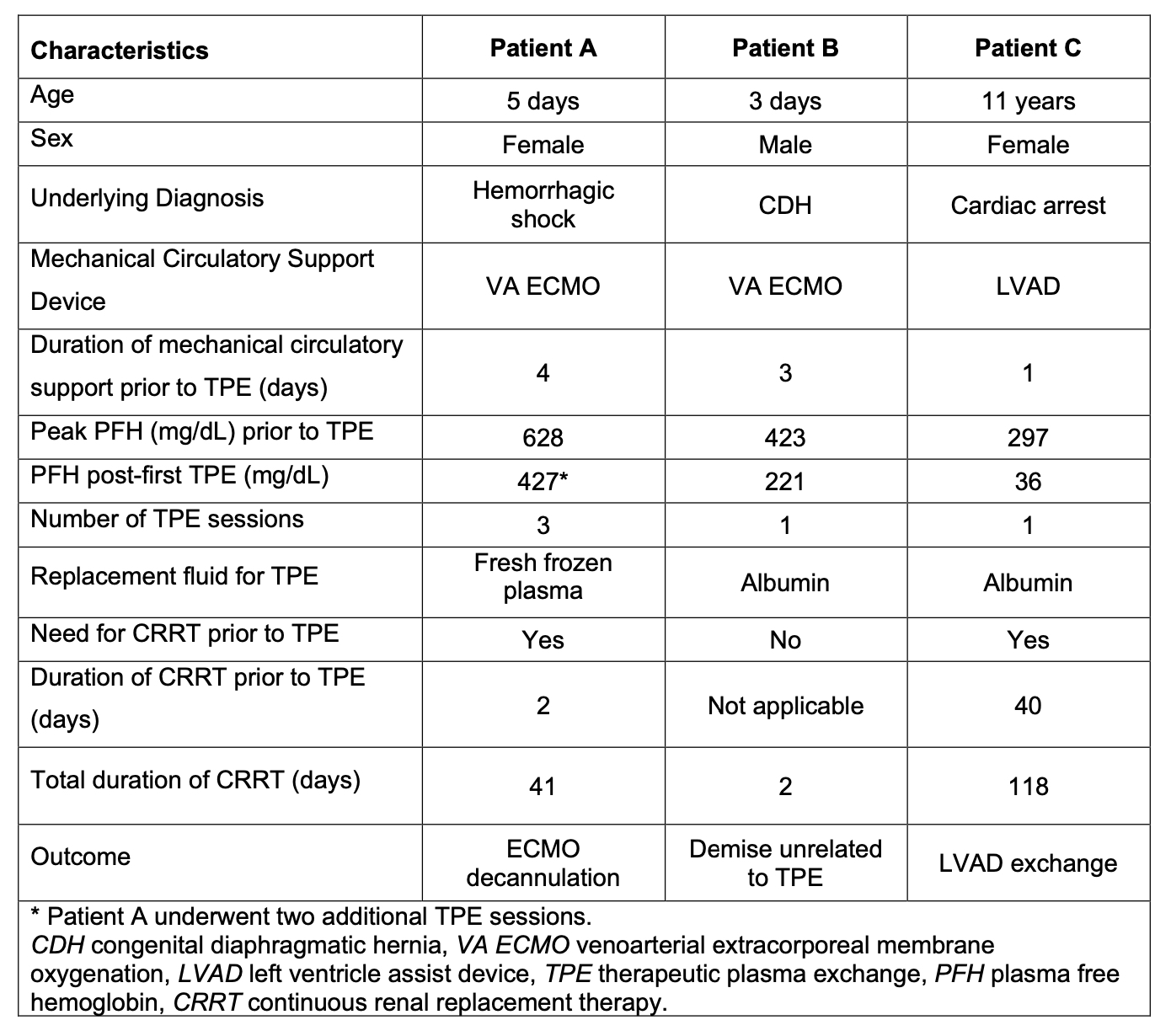
The ages of the 3 cases were: Patient A, 5 days; Patient B, 3 days; Patient C, 11 years (Table 1). Both neonatal patients were on an extracorporeal membrane oxygenation (ECMO) device at the time of rise in PFH, while the third patient had a left ventricle assist device (LVAD). All patients received continuous renal replacement therapy (CRRT) for AKI and/or fluid overload. TPE in all patients was performed using membrane filtration with Prismaflex device. The mean peak PFH level at time of initiation was 449.3 mg/dL (range 297-628 mg/dL) and the mean level after the first TPE session was 228 mg/dL (range 36-427 mg/dL). Patient A underwent three sessions of TPE prior to clinical improvement and ECMO decannulation. Patient B had clinical deterioration unrelated to the TPE procedure and underwent only a single session. Patient C had persistent hemolysis requiring LVAD exchange which led to improvement in PFH. No TPE-related complications were observed.
Conclusion(s):
TPE was safely used to reduce severely elevated PFH levels in three pediatric patients with risk factors for significant tissue toxicity. The impact on clinical outcomes was less clear in this case series. Given the risks of elevated PFH levels, additional studies are needed, along with guidelines on the appropriate use of apheresis for mechanical red cell hemolysis.