Breastfeeding/Human Milk
Breastfeeding/Human Milk 4: Breastfeeding and Milk Provision
42 - Improving Lactation Resources for Residents and Fellows at a Pediatric Hospital
Publication Number: 42.202

Sabrina Ben-Zion, MD (she/her/hers)
Associate Program Director, Pediatric Residency
Akron Children's Hospital
Akron Children's Hospital
Akron, Ohio, United States
Presenting Author(s)
Background:
In 2019, the Accreditation Council of Graduate Medical Education (ACGME) added a new core requirement to the common program requirements to ‘‘ensure healthy and safe learning and working environments that promote resident/fellow well-being and provide for clean and private facilities for lactation that have refrigeration capabilities, with proximity appropriate for safe patient care.’’ While Akron Children’s Hospital had lactation spaces, they were not conveniently located to resident workspaces, nor did they have refrigeration. Residents were often transporting breast pumps back and forth to the hospital and using cooler bags to store pumped milk for their entire shifts.
Objective:
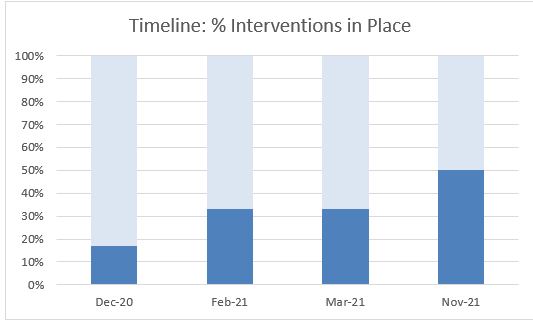
The global aim of this project was to improve support of residents and fellows who breastfeed. Specifically, we aimed to increase interventions in place to support lactating trainees from 0% to 50% by March 30, 2021.
Design/Methods:
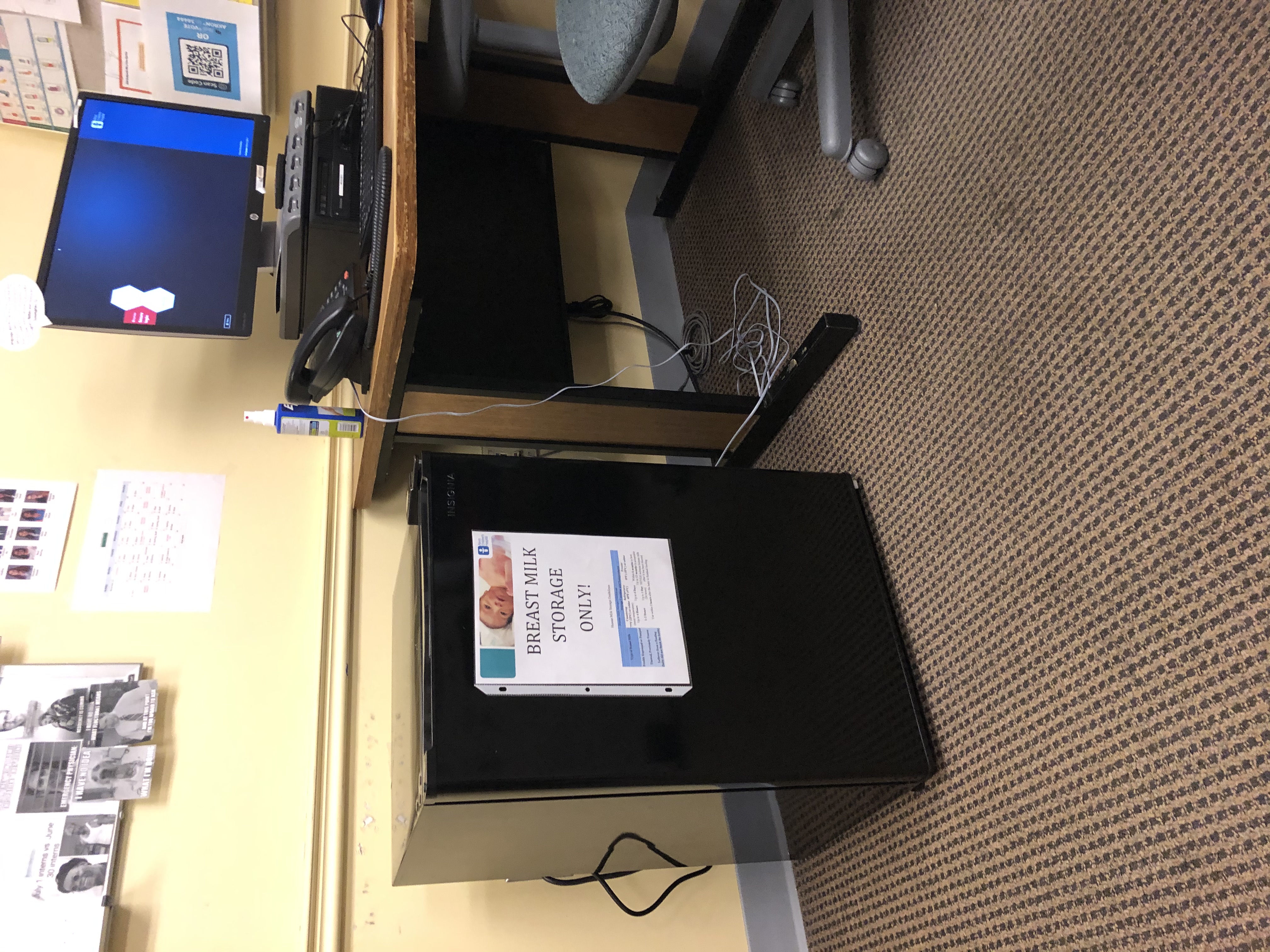
We used the IHI quality improvement methodology and tools for this project. We assembled a multidisciplinary work group starting in July of 2020 that included residency faculty, a lactation consult, a QI specialist, nursing leadership, residents, and our designated institutional official. We elicited feedback from current and past residents who were either breastfeeding or had breastfed about barriers to successful breastfeeding within the institution. From this, we created a key driver diagram which informed our interventions including (1) lactation spaces close to clinical duties, (2) breastmilk storage in resident and fellow workspaces, (3) on-site breast pumps, (4) resource packet for lactating trainees (5) trainee specific lactation policy, (6) adjust clinical schedules to allow time for pumping. We used PDSA cycles to guide next steps and created a compliance checklist to inform our progress.
Results:
We did not reach our goal of 50% of resources in place by March 2021 but currently are at 50%. Challenges to success have been securing financial support from stakeholders and longer than usual wait times for construction supplies. We have started to track utilization of lactation spaces and refrigerators and future direction includes eliciting trainee satisfaction with available resources.
Conclusion(s):
Implementation of QI methodology has ensured compliance with ACGME requirements and increased support of breastfeeding trainees at our pediatric institution..jpg)