Neonatal GI Physiology & NEC
Neonatal GI Physiology & NEC 5: Predicting Necrotizing Enterocolitis, Gut Health, and Oral Feeding
106 - PROGRESSION OF ENTERAL FEEDING VOLUMES IN EXTREMELY PREMATURE INFANTS IN THE ‘CONNECTION TRIAL’
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 106
Publication Number: 106.237
Publication Number: 106.237
Jonas Rastad, Infant Bacterial Therapeutics, Stockholm, Stockholms Lan, Sweden; Staffan Stromberg, IBT, Stockholm, Stockholms Lan, Sweden; Marcus Thuresson, Infant Bacterial Pharmaceuticals, Uppsala, Uppsala Lan, Sweden; Josef Neu, University of Florida, Gainesville, FL, United States; Anders Kronstrom, Infant Bacterial Therapeutics, Stockholm, Stockholms Lan, Sweden
- JN
Josef Neu, MD
Professor
University of Florida
Gainesville, Florida, United States
Presenting Author(s)
Background: Numerous clinical features may prevent advancement of enteral feeding in extremely low birth weight (ELBW) infants.
Objective: Herein we correlate clinical features with the time to reach certain levels of enteral feeding in ELBW infants.
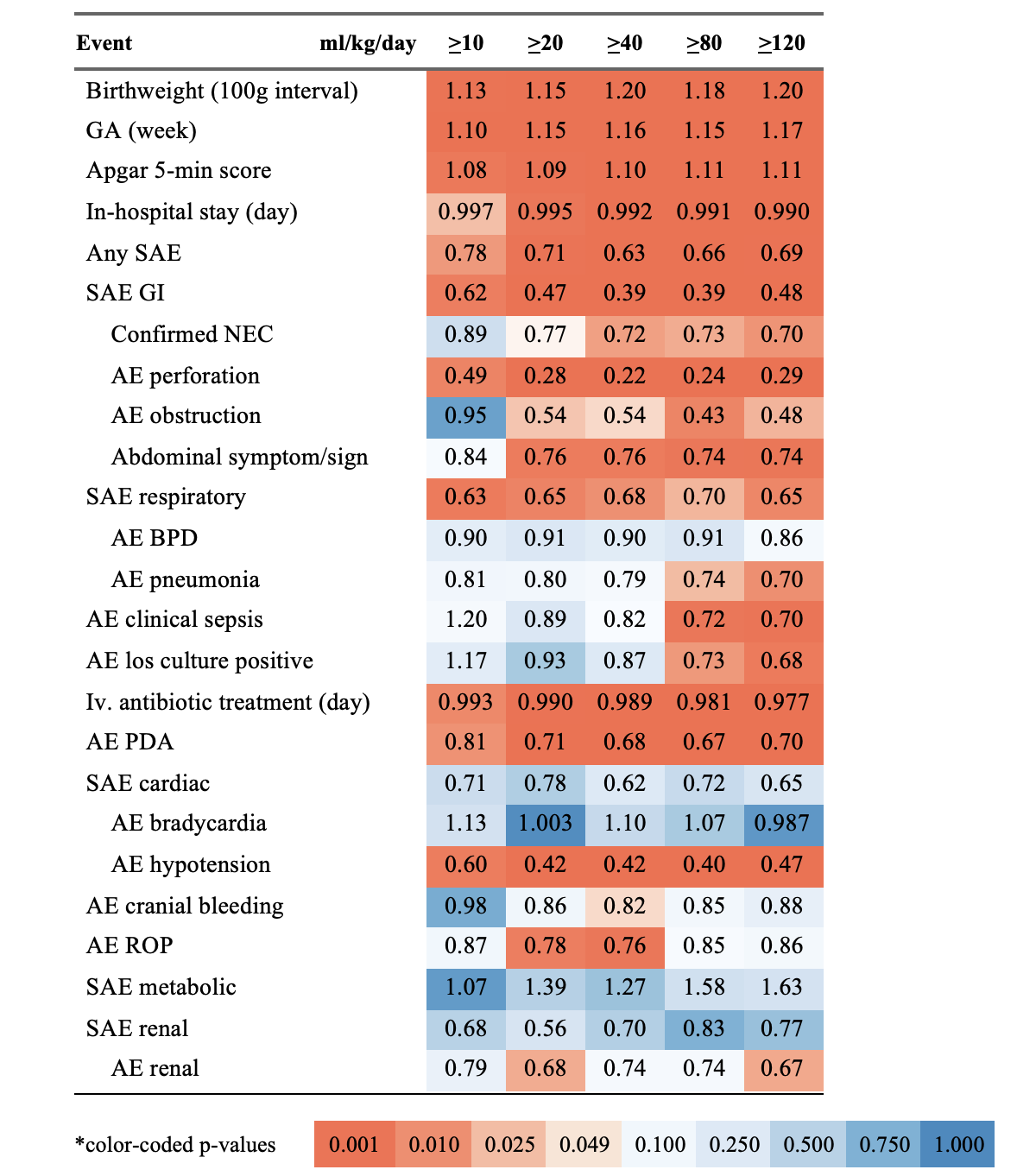
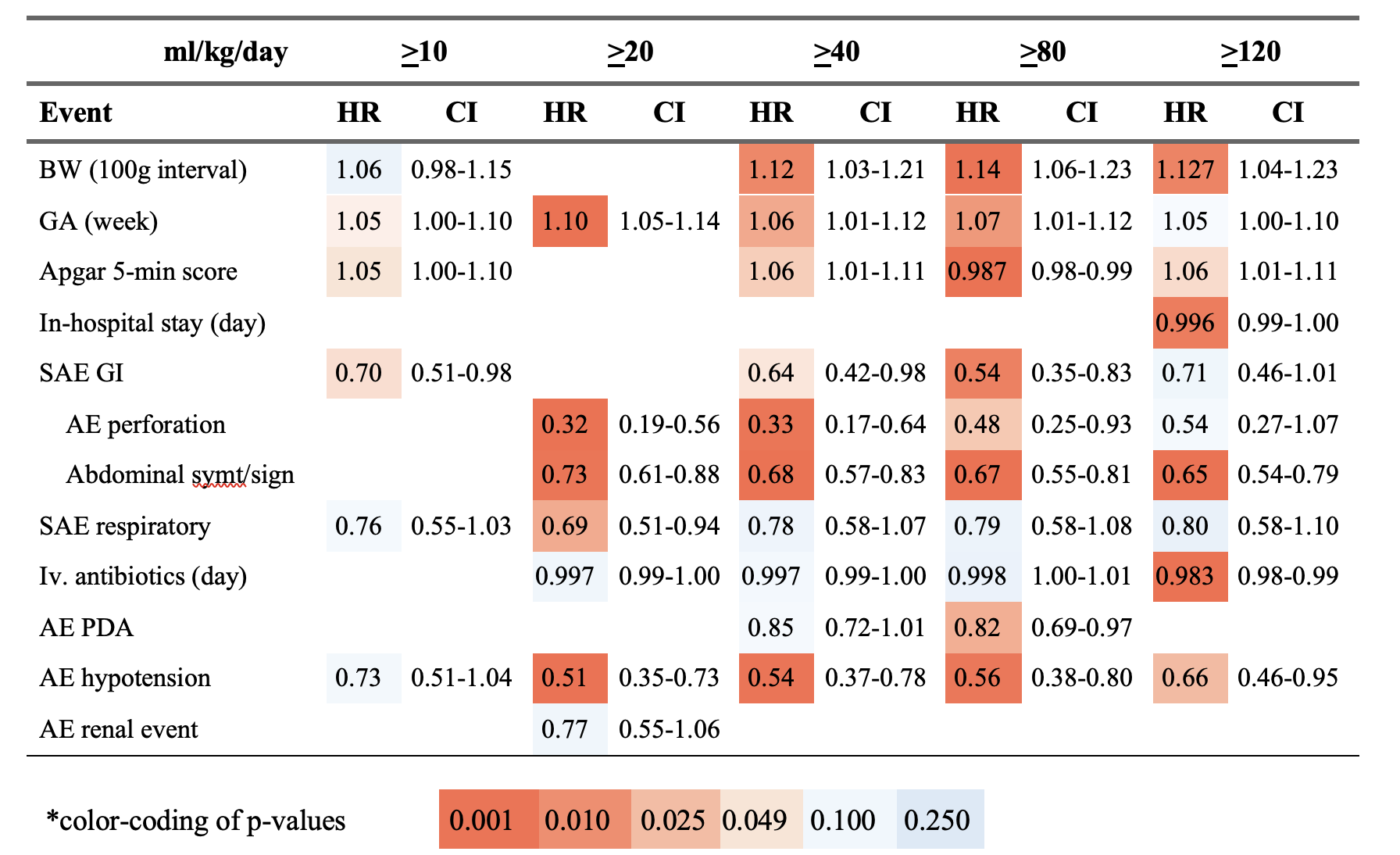
Design/Methods: 641 infants of 510-1000g (mean, 847g) birthweight (BW) and gestational age (GA) 23-32 weeks (mean, 27w) at birth were analyzed for total daily (td) enteral intakes and for any association of 25 clinical variables with the time from birth to total intakes of >10, 20, 40, 80 and 120 ml/kg/day. The infants are participants in the ongoing ‘Connection Trial’ and were randomized 1:1 to IBP-9414 (L. Reuteri of pharmaceutical grade) or placebo. All analyses were performed without knowledge on treatment group allocation of the infants. Uni- and multivariable Cox regression models were used to calculate hazard ratios (HR) with 95% confidence intervals. A low HR signifies a reduced chance of reaching the desired td-volumes.
Results: Daily feeding volumes were highly variable (Fig. 1). It took one fourth of infants 5 days or more to reach 10 ml/ and the median age at reaching 120 ml/kg was 14 days (Fig. 2, Table 1). Univariate analyses (Table 2) showed the lowest HR for reaching the td-volumes associated with gastrointestinal (GI) serious adverse events (SAEs), GI perforation and GI obstruction, necrotizing enterocolitis, respiratory compromise, persistent ductus arteriosus and hypotension (HR, 0.22-0.81). One-week higher GA, 100 g BW and 5-min Apgar score at birth associated with an 8%-20% increased chance of attaining any of the td-volumes. Multivariable analyses (Table 3) with a stepwise approach showed independent effects on the time to the td-volumes for BW, GA, Apgar score, GI SAEs including perforation, abdominal symptoms/signs, respiratory compromise, days on iv. antibiotics and hypotension.
Conclusion(s): Initiation and progression of enteral feeding in the currently investigated infants were highly variable and associated statistically to a range of clinical variables. Although these associations do not demonstrate causality, they suggest the relative impact these variables may have in the current clinical decision-making on the advancement of enteral feeding volumes in ELBW infants.
.png)
