Neonatal Hematology & Bilirubin Metabolism
Neonatal Hematology & Bilirubin Metabolism 2: Hematology
139 - Storage age and irradiation of packed red blood cells and its relation to cell-free hemoglobin levels
Publication Number: 139.239

Kashif Iqubal, MD (he/him/his)
Fellow (Neonatal-Perinatal Medicine)
Hassenfeld Children's Hospital at NYU Langone
Jersey city, New Jersey, United States
Presenting Author(s)
Background:
Pack Red Blood Cells (PRBC) are stored for different durations of time before they are transfused to patients, including neonates. Hemolysis and metabolic changes that can occur during storage have been proposed as factors that may lead to transfusion-related morbidities in preterm neonates such as transfusion-associated gut injury, retinopathy of prematurity, and intraventricular hemorrhage (IVH). Irradiation of PRBC units increases hemolysis. Cell-free Hemoglobin (cHb) released after hemolysis is a potent scavenger of nitric oxide and is believed to accumulate in PRBC bags with storage.
Objective: To determine any relationship that may exist between the storage age of PRBC units and time since unit irradiation in comparison to cHb levels found in the PRBC being transfused to preterm infants.
Design/Methods: Prospective observational study. Premature infants born between 25-31 weeks gestation and 500-1500 grams of weight were included in the study. Infants with congenital heart disease, major congenital malformations, abdominal surgery, and grade III or IV IVH were excluded. Levels of cHb in the PRBC unit was measured by a portable cHb analyzer prior to the transfusion starting. Student t-test and Pearson correlation test were used for statistical analyses
Results:
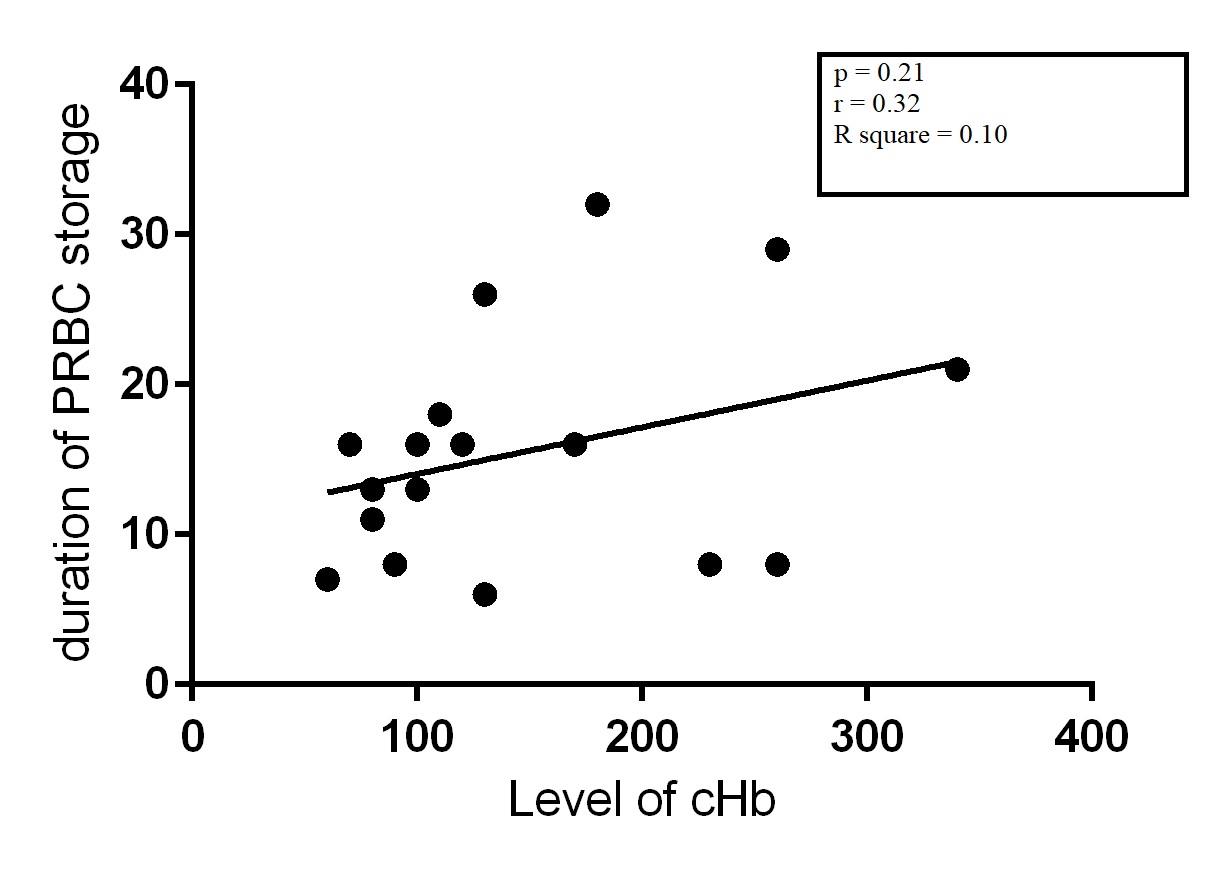
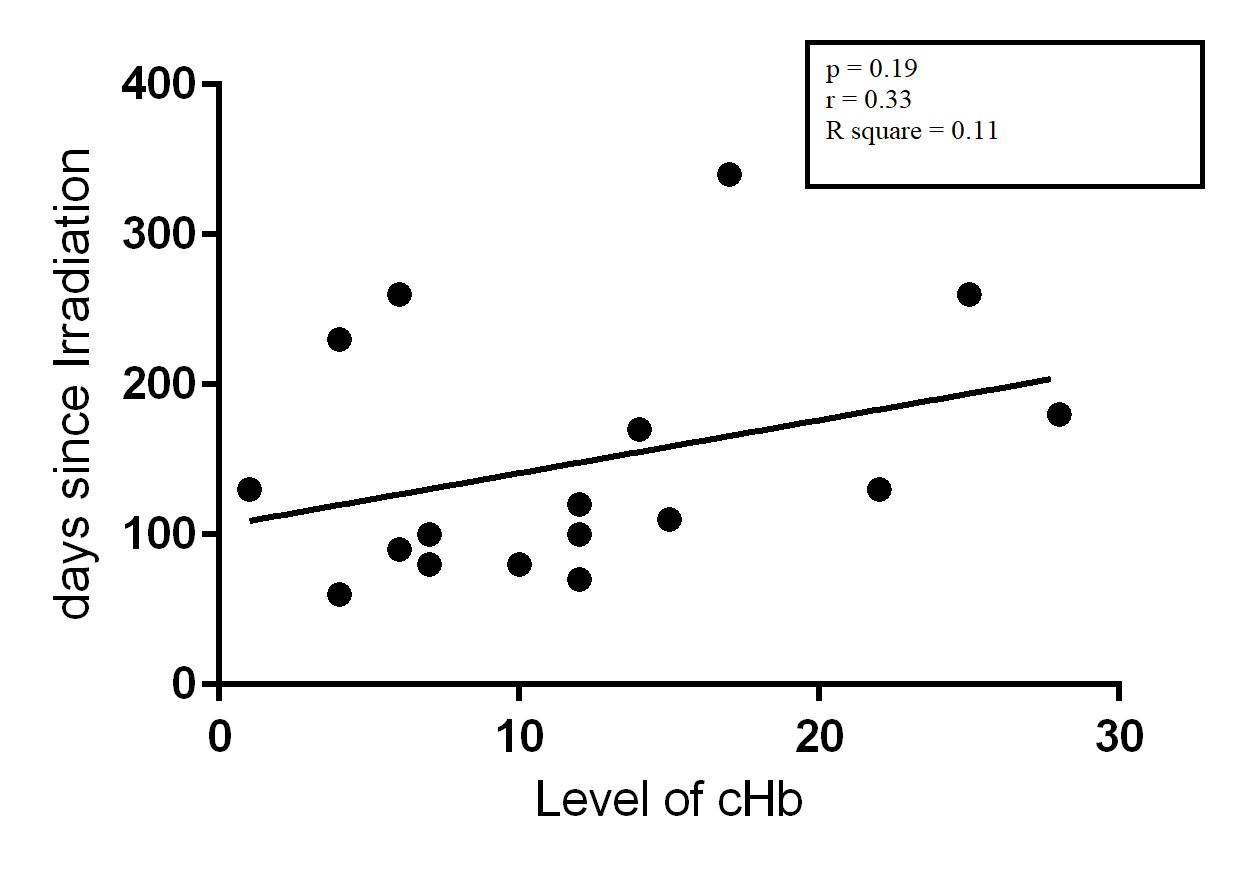
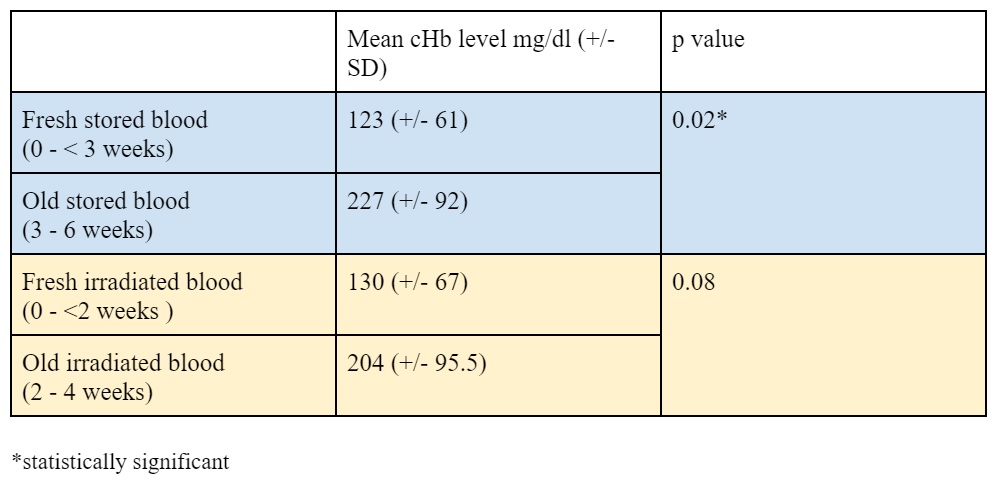
17 transfusions monitored. The mean duration of storage of PRBC was 15.4 ± 7.7 days and the mean number of days from irradiation to transfusion was 11.8± 7.6 days. The mean cHb level found in the transfused PRBC blood was 147.66 ± 80.6 mg/dl. Although there was an increase in cHb levels with an increase in storage time, the correlation was not statistically significant (p = 0.21, R2= 0.10). Levels of cHb also increased with increasing duration after irradiation but the correlation between duration since irradiation and the level of cHb was also not significant (p= 0.19, R2= 0.11). When examining freshly stored blood (< 3 weeks) to older blood (3 weeks - 6 weeks), there was significantly lower cHb levels, 123± 61 mg/dl vs 227 ± 92 mg/dl, (p= 0.02) in the fresher blood [Table 1]. Similarly looking into freshly irradiated (< 2 weeks) to older irradiated blood (2-4 weeks), we did see lower mean cHb levels, in freshly irradiated blood, 130 ± 67 mg/dl vs 204 ± 95.5 mg/dl but the difference was not quite statistically significant (p = 0.08) [Table 1].
Conclusion(s):
Levels of cHb appear to increase with longer duration of storage and longer time since irradiation. Blood banks and clinicians involved in neonatal transfusions could consider this before transfusing PRBCs in this population.