Nephrology: Dialysis
Nephrology 1: AKI
257 - Characteristics and Outcomes of Continuous Renal Replacement Therapy in Pediatric Sepsis: A Report from Worldwide Exploration of Renal Replacement Outcomes Collaborative in Kidney Disease (WE-ROCK)
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 257
Publication Number: 257.25
Publication Number: 257.25
Natalja L. Stanski, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Denise Hasson, New York University Grossman School of Medicine, New York, NY, United States; Erin K. Stenson, Children's Hospital Colorado, Aurora, CO, United States; Katja M. Gist, Children's Hospital Medical Center (Cincinnati), Cincinnati, OH, United States; JANGDONG SEO, Cincinnati Children's Hospital, Bloomington, IN, United States; Dana Fuhrman, UPMC Childrens Hospital of Pittsburgh, Pittsburgh, PA, United States

Natalja L. Stanski, MD (she/her/hers)
Assistant Professor of Pediatrics
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Sepsis is common in the pediatric intensive care unit (PICU) and is associated with morbidity and mortality. Acute kidney injury (AKI) is a common complication that increases the risk of poor outcomes. As there are no disease-modifying therapies for sepsis-associated AKI, continuous renal replacement therapy (CRRT) is often needed. Limited data exist regarding characteristics and outcomes of children with sepsis requiring CRRT.
Objective: We aimed to (1) describe the characteristics and outcomes of children with sepsis requiring CRRT compared to those without sepsis, and (2) identify factors associated with the development of Major Adverse Kidney Events at 90 days (MAKE-90) in children with sepsis requiring CRRT.
Design/Methods: A secondary analysis of WE-ROCK, an international (7 countries), multicenter (32 centers), retrospective study of subjects aged 0-25 years treated with CRRT for AKI or fluid overload (FO) from 2018-2021. Patients had sepsis if they met ≥2 SIRS criteria and were treated for a known/suspected infection at CRRT start. Patients suffered MAKE-90 if they had any of the following at 90 days: mortality, persistent kidney dysfunction (serum creatinine ≥ 200% baseline), or RRT dependence. Children with sepsis who suffered MAKE-90 were compared to those who did not to assess for factors associated with MAKE-90.
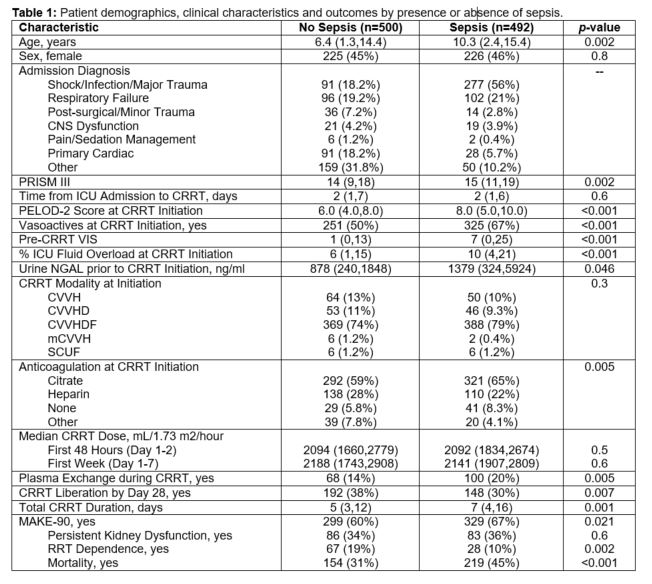
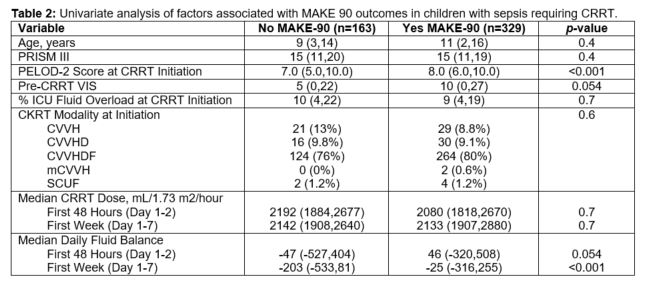
Results: Among 992 patients, 492 (49.6%) had sepsis at CRRT start. Compared to children without, those with sepsis had higher PRISM III (15 vs. 14, p=0.002), and at CRRT start, had higher PELOD-2 (8 vs. 6, p< 0.001), higher vasoactive inotrope scores (VIS) (7 vs. 1, p< 0.001), and greater %FO (10% vs. 6%, p< 0.001) (Table 1). There were no differences in initial CRRT modality or prescription between groups. Children with sepsis were less likely to liberate from RRT by 28 days (30% vs. 38%, p=0.007), had longer duration of CRRT (7 vs. 5 days, p=0.001), suffered more MAKE-90 (67% vs. 60%, p=0.021) and mortality (45% vs. 31%, p< 0.001); however, they were less likely to be RRT dependent at 90 days (10% vs. 19%, p=0.002) (Table 1). On univariate analysis, children with MAKE-90 had higher PELOD-2 prior to CRRT start and more positive daily fluid balance over the first 7 days of CRRT (Table 2).
Conclusion(s): Septic children requiring CRRT have unique clinical characteristics and outcomes, including higher rates of mortality and MAKE-90, compared to those without sepsis. More positive net daily fluid balance over the first week of CRRT may be associated with MAKE-90 in septic children, though further analysis is needed.