Immunizations/Delivery
Immunizations/Delivery 1
611 - Emergency Departments: An Opportunity to Address Pediatric Influenza Vaccine Disparities
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 611
Publication Number: 611.224
Publication Number: 611.224
Rebecca J. Hart, University of Louisville/Norton Children's Medical Group, Louisville, KY, United States; Yana B. Feygin, University of Louisville School of Medicine, Louisville, KY, United States; Suchitra Rao, University of Colorado School of Medicine, Aurora, CO, United States; Shannon H.. Baumer-Mouradian, Medical College of Wisconsin, Milwaukee, WI, United States

Rebecca J. Hart, MD, MSc (she/her/hers)
Assistant Professor, Associate Program Director
University of Louisville/Norton Children's Medical Group
Louisville, Kentucky, United States
Presenting Author(s)
Background: Influenza vaccination (InfV) rates in Black children (49%) trail behind White (60%) and Hispanic children (59%). Emergency department (ED) based InfV programs may address pediatric vaccine disparities; however, little is known about pediatric ED InfV programs.
Objective: To describe the reach and effectiveness of InfV practices in pediatric EDs, and identify program facilitators and barriers.
Design/Methods: We conducted a cross-sectional study involving a survey of pediatric ED physicians. Using a 5-point Likert scale, we assessed which EDs offer InfV to children, number of vaccines administered per year, and program facilitators/barriers. Descriptive statistics assessed the proportion of EDs offering InfV and associated factors. Chi-square tests compared facilitators and barriers among “high performers” (administered ³ 50 InfV/year), “low performers” (administered < 50 InfV/yr), and non-vaccinators (no InfV). Multilevel regression modeling investigated the association between each barrier/facilitator and offering InfV, adjusting for clustering by facility.
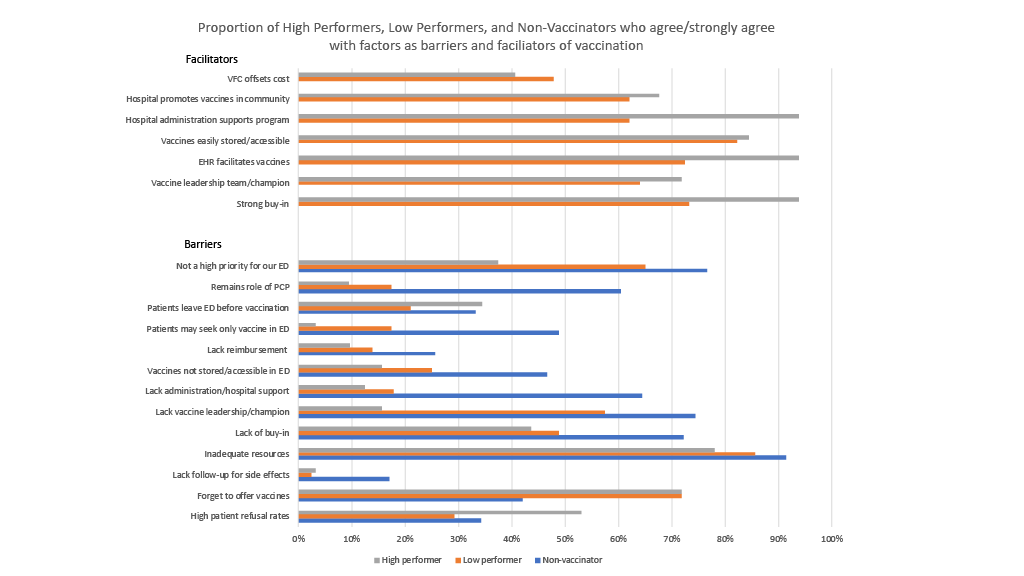
Results: We surveyed physicians from 166 EDs; 142 respondents represented 61 (37.3%) EDs. Most EDs were in large, academic, freestanding children’s hospitals in urban settings, and 28 (45.9%) manage >60% patients with Medicaid (Table 1). Only 27 EDs (44.3%) offer one or more InfV/yr. Of these, nine programs (33.3%) were “high performers” ( >50 InfV in the past year); 4 were “model programs” ( >1000 InfV). High performers were more likely than low performers to have a workflow for offering InfV (78% vs. 33%), but this was not statistically significant (p = 0.077). Common facilitator themes included: strong buy-in from providers, electronic health record facilitation, hospital administration support, ease of storage/accessibility, and having a leadership team/champion (Fig 1). Non-vaccinators commonly listed a lack of these themes as barriers. In regression analysis, lack of hospital/administration support (OR 0.0000000002, p < 0.0001) and belief that vaccination is the PCP’s role (OR 0.0000000003, p < 0.0001) were associated with decreased odds of offering InfV. There were 27 (44.3%) EDs interested in establishing or growing InfV programs.
Conclusion(s): Over half of EDs do not currently offer pediatric infV and fewer have an ED vaccination workflow. Addressing identified barriers/facilitators to develop InfV programs in EDs has potential to improve vaccination rates. We are poised to develop a model ED vaccination workflow that addresses missed opportunities to vaccinate children from minority and underserved backgrounds.
.png)