Neonatal Hematology & Bilirubin Metabolism
Neonatal Hematology & Bilirubin Metabolism 1: Bilirubin
118 - Hemoglobin and hematocrit in extremely premature infants exposed to hypertensive disorders of pregnancy
Publication Number: 118.238

Daniela Villegas Martinez, MSc
Postgraduate student
McGill University Faculty of Medicine and Health Sciences
Montreal, Quebec, Canada
Presenting Author(s)
Background:
The association between hypertensive disorders of pregnancy (HDP) and red blood cell (RBC) lineage trends remain to be explored in extreme premature infants. We were interested in evaluating the impact of HPD in prematurity on hemoglobin (Hgb) / hematocrit (Hct) at birth, trends during neonatal hospitalization and frequency of packed red blood cells (pRBC) transfusions.
Objective:
Retrospective study of infants born < 29 weeks, between 2015 and 2019. Hgb/Hct were collected on initial complete blood count, at 2 weeks, 32 weeks and 36 weeks. We examined the association between HDP and Hgb/Hctt at each time-point, and the frequency/volume of pRBC transfusions (Figure 1).
Design/Methods: Retrospective study of infants born < 29 weeks, between 2015 and 2019. Hgb/Hct were collected on initial complete blood count, at 2 weeks, 32 weeks and 36 weeks. We examined the association between HDP and Hgb/Hctt at each time-point, and the frequency/volume of pRBC transfusions (Figure).
Results:
296 extremely premature infants were included, of which 43 were exposed to HDP. HDP infants were of smaller birth weight (730 (620 - 850) vs 890 (720 - 1090) grams, p=0.0001), but of similar gestational age (26.5 (1.3) vs 26.2 (1.6), p=0.25). They had similar rates of delayed cord clamping, phototherapy and intraventricular hemorrhage. They had a higher Hgb/Hct, and a higher prevalence of polycythemia (hemoglobin >160 g/L (17% vs 40%, p=0.002)) at birth (Table 1). Values on the following time points were similar between groups (Table 1, 2 & Figure ). Infants exposed to HDP were more frequently exposed to pRBC transfusions (86% vs 65%, p=0.005) and, when exposed, to a larger volume (58 (40 - 103) vs 40 (20 – 80) mL, p=0.03). Mixed effect model demonstrated no association between HDP and hemoglobin trends during hospitalization.
Conclusion(s):
Despite higher hemoglobin/hematocrit at birth, extremely preterm infants exposed to HDP have increased frequency/volume of pRBC transfusion to maintain similar trends throughout hospitalization. 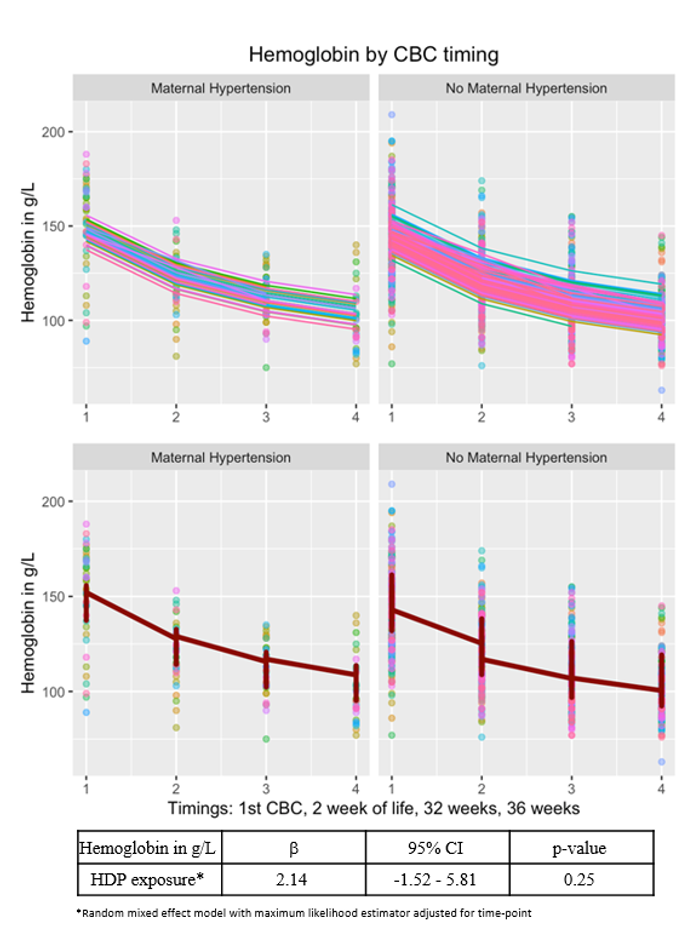
.png)
.png)
