Neonatal General
Neonatal General 5: COVID, Infections Diseases
702 - Evaluation of Routine Immunization Administration and Reactogenicity in Preterm Infants
Publication Number: 702.233

Ferras Bashqoy, PharmD, BCCCP, BCPPS (he/him/his)
NICU Clinical Pharmacy Specialist
NYU Hassenfeld Children's Hospital
New York, New York, United States
Presenting Author(s)
Background:
Immunization of preterm infants has been the subject of debate due to concerns for reactogenicity and reduced immunogenicity. Although the American Academy of Pediatrics recommends medically stable infants receive routine vaccination per schedule, a 2018 survey revealed that the majority of neonatologists delayed 2-month vaccinations and spread them over ≥ 2 days. Hassenfeld Children’s Hospital underwent a practice change 1/2021 from administering vaccinations on separate days to administering on a single day at 2 months postnatal age.
Objective:
To evaluate the relationship between routine vaccination [Pediarix(DTaP-HepB-IPV)/Hib/PCV13] and cardiorespiratory events in preterm infants when administering all vaccines at once vs. one per day.
Design/Methods:
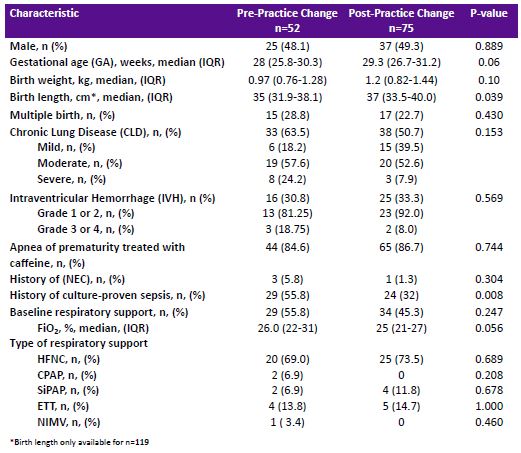
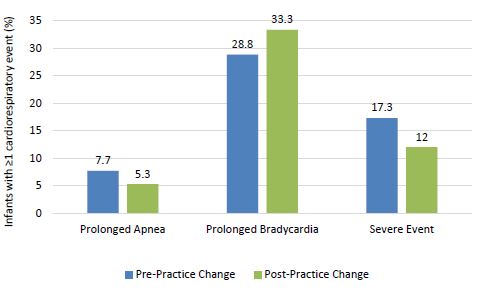
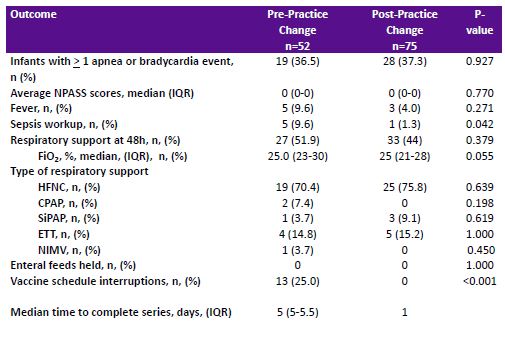
This IRB approved retrospective chart review included preterm NICU patients receiving 2-month vaccines between 12/2019 to 9/2022. The primary outcome was to compare the incidence of cardiorespiratory events (prolonged bradycardia, prolonged apnea and severe events) within 48 hours of vaccination. Secondary outcomes include a comparison of sepsis workups, incidence of fever, and pain scores between groups. Descriptive statistics, Chi‐square, Fishers’ exact test, and Wilcoxon rank sum statistics were performed.
Results:
There were 127 patients included with 52 in the pre-practice change group and 75 patients in the post-practice change group. Baseline characteristics and baseline apnea/bradycardia events were similar between groups except there were more infants in the pre-practice change group with a history of culture--proven sepsis (55.8 vs 32%, p=0.008) and shorter birth length (35 cm vs. 37 cm, p=0.039). The incidence of cardiorespiratory events (prolonged bradycardia, prolonged apnea and severe events) within 48 hours of vaccination were not different between groups (p=0.715; 0.592; and 0.399 respectively). A greater percentage of infants in the pre-practice change cohort had a vaccine schedule interruption or underwent a sepsis workup within 48 hours of immunization. A greater percentage of infants in the post-practice change cohort received a one time dose of acetaminophen as a supportive care agent.
Conclusion(s):
Administration of routine 2-month vaccinations all at once was not associated with increased cardiorespiratory events or adverse effects in preterm infants