Neonatal General
Neonatal General 4: GI-Nutrition-Growth
686 - Prevalence and management of feeding problems -in Extremly Low Birth Weight and Very Low Birth Weight premature babies using Fiberoptic Evaluation of Swallowing
Publication Number: 686.232
- MS
Mustafa Suterwala, MD (he/him/his)
Medical Director
Pediatrix Medical Group and Baylor University Medical Center
Dallas, Texas, United States
Presenting Author(s)
Background: Increasing rates of survival of premature babies has resulted in increased attention to feeding problems in this vulnerable group. Feeding problems have long-term effects on growth, development, and lung function. Full oral feeding with adequate growth is an essential criterion for hospital discharge. The pressure to decrease length of stay in hospital results in parent and provider frustration, use of poor feeding practices, including force feeding, and increased rate of gastronomy tube usage.
Objective:
We have pioneered a multidisciplinary approach with a team of neonatologist, nurse, speech pathologist (SP), occupational therapist (OT), and nutritionist working together to address feeding problems. We use an individualized approach based on a clinical feeding evaluation, standardized feeding tool including Infant Driven Feeding Scales (IDFS) and Fiberoptic Evaluation of Swallowing (FEES), to diagnose and treat feeding problems in premature babies. Feeding problems are dynamic and continue to evolve as the infant matures, requiring ongoing assessment, intervention, and revaluation to achieve optimum feeding outcome.
Design/Methods: The Study population includes all babies admitted at less than 28 weeks gestation at tertiary care NICU from 2016-2022, which were retrospectively analyzed. All the babies had a clinical feeding evaluation by OT and SP. Daily assessment was done using IDFS. Infants were followe up until full oral feeding was achieved. The team decided if an infant meet criterion for FEES at or after 38 weeks. Feeding strategies based on FEES were implemented and evaluated for feeding progress.
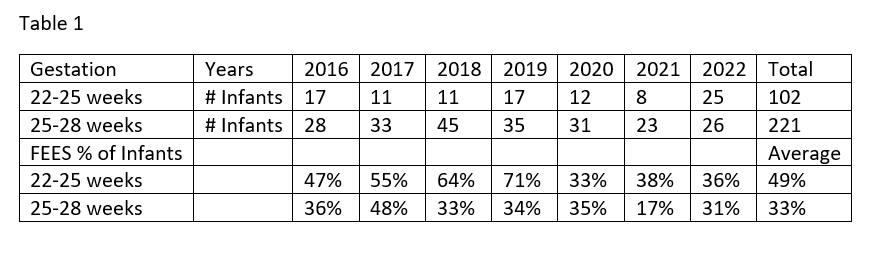
Results: Feeding problems were identified in 49% babies born between 22-25 weeks and 33% born between 25–28-week, as shown Table 1. This is higher than the general reported incidence of 20-26% amongst NICU graduates. 11% infants had anatomical defects requiring ENT consult and follow-up bronchoscopy. 30% of infants, required assisted feeding techniques, feeding position, slow flow nipples, or exclusive breast feeding and 59% diagnosed with laryngeal aspiration or penetration requiring bolus management with pre thickened formula, or Gelmix if breast milk was available to achieve adequate oral intake. Gastrostomy tubes rates in this group were 1.2%.
Conclusion(s): The incidence of feeding problem in the very premature is high, with almost half the population requiring some form of intervention. A multidisciplinary approach using FEES as diagnostic tool was effective in diagnosis and management. Use of thickened feeds and assistive feeding strategies resulted in a decrease in the need for gastrostomy tubes.