Neonatal GI Physiology & NEC
Neonatal GI Physiology & NEC 5: Predicting Necrotizing Enterocolitis, Gut Health, and Oral Feeding
103 - Prevention of Necrotizing Enterocolitis in Very Preterm Infants: A Quality Improvement Initiative
Publication Number: 103.237
.jpg)
Tom Sproat, MBChB MRCPCH MD (he/him/his)
Neonatal-perinatal medicine fellow
University of Calgary Cumming School of Medicine
Calgary, Alberta, Canada
Presenting Author(s)
Background:
Necrotising Enterocolitis (NEC) is a leading cause of morbidity and mortality in preterm infants.
The pathogenesis of NEC is multifactorial. Intestinal immaturity, highly immunoreactive intestinal mucosa and abnormal microbial colonization are factors that predispose to NEC.
A previous quality improvement (QI) project in our unit aimed at improving breastmilk feeding had lead to a reduction in NEC to 4.7%. We aimed to further reduce the rate of NEC using multiple targeted interventions.
Objective:
To reduce the incidence of necrotizing enterocolitis (NEC) among infants born < 33+0 weeks gestational age to ≤2%.
Design/Methods:
This QI initiative was conducted across 5 neonatal units. A multidisciplinary team developed key drivers for NEC. Targeted interventions included strategies to; increase mother’s own milk (MOM), improve compliance with feeding regimens, standardize management of feeding intolerance, prevent intestinal microbial aberrations and alter feeding guidelines (conservative feeding during blood transfusion and treatment of patent ductus arteriosus) (Figure 2).
The outcome measure was rate of NEC (≥Bell's stage 2). Process measures included MOM feeding at hospital discharge, difference between actual and expected (based on feeding regimen) time to reach full enteral feeds, lowest hemoglobin level, and duration of initial empiric antibiotics. Balancing measures were growth velocity, rate of blood transfusion, duration of parenteral nutrition, length of hospital stay, and late-onset sepsis.
Data were analyzed with statistical process control charts. The pre-intervention period was from January 2013 to June 2016, implementation period was from July 2016 to December 2018, and sustainment period was from December 2018 to December 2021.
Results:
We included 2787 infants born at ≤32 weeks’ gestation (1105 pre-intervention, 763 during intervention, and 919 in sustainment) (Table 1).
Incidence of NEC decreased from 5.6% to 1.9% (Figure 1). Process measures indicated increased MOM feeding at discharge, improved compliance with feeding regimens, increased lowest hemoglobin levels, and shorter duration on initial empiric antibiotics. Balance measures showed improved weight Z-scores, shorter duration on parenteral nutrition, and increased rate of blood transfusion (Table 1).
Conclusion(s):
QI initiatives to increase MOM, improve compliance with feeding regimens, conservative feeding guidelines during blood transfusion and treatment of patent ductus arteriosus, and prevention of intestinal microbial aberrations were associated with reduced incidence of NEC to < 2%, which was sustained for 3 years.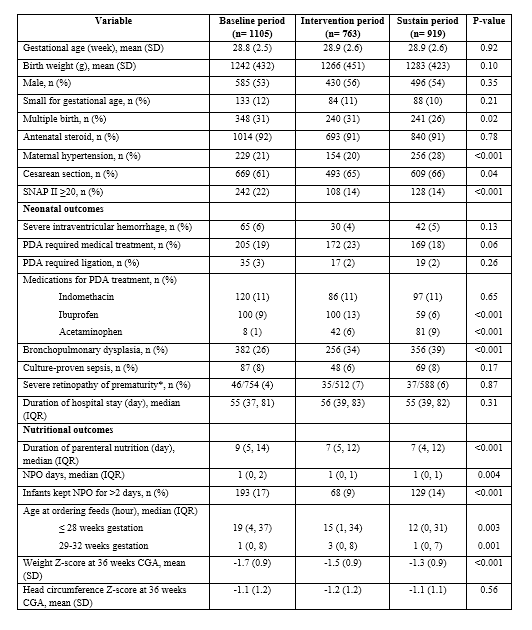
.png)
.png)
