Nephrology: Dialysis
Nephrology 3: Dialysis and Diversity and Equity in Kidney Health
285 - Peritonitis risk factors in children receiving chronic peritoneal dialysis
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 285
Publication Number: 285.252
Publication Number: 285.252
Heather L. Wasik, State University of New York Upstate Medical University, Syracuse, NY, United States; Troy Richardson, Children's Hospital Association, Lenexa, KS, United States; Raj P. Munshi, Seattle Childrne's, Seattle Children's, WA, United States; Mahima Keswani, Ann and Robert H. Lurie Childrens Hospital of Chicago; Northwestern Medicine, Chicago, IL, United States; Brad A. Warady, Children's Mercy, Kansas City, MO, United States; Alicia Neu, The Johns Hopkins University School of Medicine, Baltimore, MD, United States

Heather L. Wasik, MD, MHS (she/her/hers)
Pediatric Nephrologist
State University of New York Upstate Medical University
Syracuse, New York, United States
Presenting Author(s)
Background: Many recommendations regarding peritonitis prevention in international consensus guidelines are expert-opinion rather than evidence-based due to a lack of published data.
Objective: The aim of this study is to examine the impact of peritoneal dialysis (PD) catheter insertion technique, timing of gastrostomy insertion in relation to PD catheter placement, and use of prophylactic antibiotics prior to invasive procedures on the risk of peritonitis in children on PD
Design/Methods: Retrospective cohort study of children on PD using data from the SCOPE collaborative from 2011-2022. Data pertaining to laparoscopic PD catheter placement (vs open), gastrostomy placement after PD catheter placement (vs before), and no prophylactic antibiotics (vs yes) was obtained. Multivariable generalized linear mixed modeling was used to assess the relationship between each exposure and the occurrence of peritonitis.
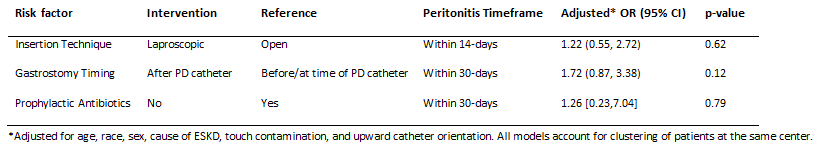
Results: There was no significant association between PD catheter insertion technique and the development of peritonitis (aOR=1.22, 95% CI 0.55-2.72, p=0.6). Patients who had a gastrostomy inserted after PD catheter placement had higher rates of peritonitis, but the difference was not statistically significant (aOR=1.72, 95% CI 0.87-3.38, p=0.12). Patients who received prophylactic antibiotics with genitourinary and gastrointestinal procedures, but not dental procedures, had lower rates of peritonitis, but the difference was not statistically significant (aOR=1.26, 95% CI 0.23-7.04, p=0.79) (Table).
Conclusion(s): PD catheter insertion technique does not appear to have a significant impact on peritonitis risk. Timing of gastrostomy placement and the use of prophylactic antibiotics following selective procedures may have some impact on peritonitis risk