Nephrology: Clinical
Nephrology 1: AKI
254 - The Association of Patient and Technical Characteristics and Survival: A retrospective analysis of the Worldwide Exploration of Renal Replacement Outcomes Collaborative in Kidney Disease (WE-ROCK)
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 254
Publication Number: 254.25
Publication Number: 254.25
Michelle C. Starr, Indiana University School of Medicine, Indinapolis, IN, United States; Huaiyu Zang, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Shanthi S. Balani, University of Minnesota Masonic Children's Hospital, Minneapolis, MN, United States; Aadil Kakajiwala, Childrens National Hospital, Washington, DC, United States; Melissa Muff-Luett, University of Nebraska College of Medicine, Omaha, NE, United States; Cara L. Slagle, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Sonia Solomon, Maria Fareri Children's Hospital at Westchester Medical Center, Valhalla, NY, United States; Rachana Srivastava, UCLA Mattel Childrens Hospital, Los Angeles, CA, United States; Eileen A. Ciccia, Washington University in St. Louis School of Medicine, St. Louis, MO, United States; Matthew Pinto, Maria Fareri Children's Hospital at Westchester Medical Center, Valhalla, NY, United States; Aaron Kessel, Cohen Children's Medical Center, New Hyde Park, NY, United States; Catherine Joseph, Baylor College of Medicine, Houston, TX, United States; Katja M. Gist, Children's Hospital Medical Center (Cincinnati), Cincinnati, OH, United States; Shina Menon, University of Washington School of Medicine, Seattle, WA, United States

Michelle C. Starr, MD MPH (she/her/hers)
Assistant Professor of Pediatrics, Department of Pediatrics, Division of Pediatric Nephrology
Indiana University School of Medicine
Indinapolis, Indiana, United States
Presenting Author(s)
Background:
There are limited large multicenter studies on epidemiology and outcomes of pediatric patients receiving continuous kidney replacement therapy (CKRT).
Objective: We aimed to describe associations between patient characteristics, initial CKRT prescription and ICU survival.
Design/Methods: The WE-ROCK study is a retrospective international multicenter study (32 centers, 7 nations) of patients aged 0-25 years treated with CKRT for Acute Kidney Injury (AKI) or Fluid Overload (FO) from 2018-21. Patients with previous dialysis dependence, ECMO utilization, or who received CKRT for non-AKI/fluid overload were excluded. Primary outcome for analysis was survival to ICU discharge, and univariate analyses were performed to assess associations.
Results:
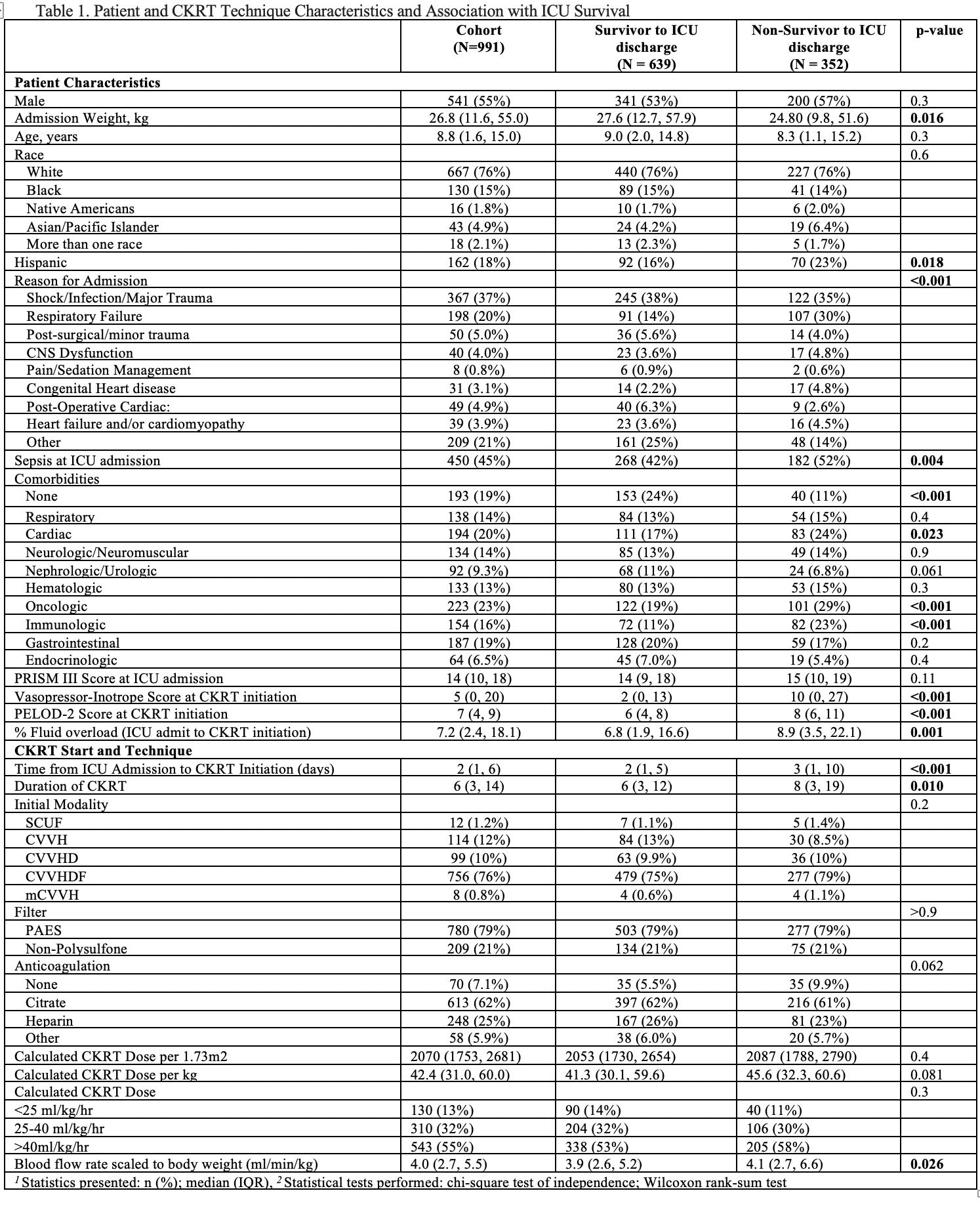
Data from 991 children were included (45% female) and 639 (64.5%) survived to ICU discharge. Ages were newborn to 25 years with a median weight of 26.8kg (IQR 11.6–55.0). The most common reason for admission was shock, infection, or trauma (37%), followed by respiratory failure (20%) and 45% had sepsis at ICU admission. Co-morbidities were seen in 81%, with oncologic (23%) and cardiac (20%) being most common.
CKRT was initiated a median of 2 days (IQR 1,6) after ICU admission and lasted a median of 6 days (IQR 3, 14). At time of CKRT initiation, patients were on average 7.2% FO. Patients that did not survive to ICU discharge were more likely to have higher degrees of FO (8.9% vs 6.8%, p=0.001), later initiation of CKRT (3d vs 2d, p< 0.001), and longer duration of CKRT (8d vs 6d, p=0.01).
The most common modality prescribed at initiation was CVVHDF (76%) with polysulfone filters (79%). Median blood flow per body weight was 4.0ml/min/kg (IQR 2.7, 5.5). Median hourly CKRT dose was 2070ml/1.73m2 or 42.4ml/kg, with most patients (55%) prescribed a dose of >40ml/kg/hr. Anticoagulation was most commonly citrate (62%) followed by heparin (25%). The most common location of catheter placement was internal jugular (66%) with size ranging from 6Fr to 14Fr. There were no differences between ICU survivors and non-survivors with regards to CKRT dose, filter type, blood flow, or anticoagulation.
Conclusion(s): This is the largest epidemiological study of patients receiving CKRT in the pediatric ICU. Sicker patients with comorbidities may have lower survival. Higher dose prescribed CKRT ( >40ml/kg) and citrate anticoagulation were common. While techniques in dialysis mode, dose, catheter size and location and anticoagulation existed in this cohort, there were no survival differences seen. Center differences may present opportunities to define best practices with future study.