Immunizations/Delivery
Immunizations/Delivery 1
608 - A Video-Based Intervention to Assess COVID-19 Vaccine Acceptability in a Pediatric ED
Saturday, April 29, 2023
3:30 PM - 6:00 PM ET
Poster Number: 608
Publication Number: 608.224
Publication Number: 608.224
Brittany G. Ebbing, University of New Mexico School of Medicine, Albuquerque, NM, United States; Lynne Fullerton, University of New Mexico School of Medicine, Albuquerque, NM, United States; Sarah E. Putnam, University of New Mexico School of Medicine, Albuquerque, NM, United States; Neehar Kundurti, University of New Mexico School of Medicine, Albuquerque, NM, United States; Walter Dehority, University of New Mexico School of Medicine, Albuquerque, NM, United States

Brittany G. Ebbing, MD, MPH (she/her/hers)
Pediatric Emergency Medicine Fellow
University of New Mexico School of Medicine
Albuquerque, New Mexico, United States
Presenting Author(s)
Background: Children have unacceptably low rates of COVID-19 vaccine uptake, ranging from 58% among 12 to 17 year-olds to 10% among those 6 months to 4 years old. Given limited access to primary care for many children, Pediatric Emergency Departments (PED) have been suggested as novel settings for COVID-19 vaccine administration.
Objective: Our study tested the following hypothesis: Among parents of children presenting to a PED, a brief video educational intervention will be associated with an increase in COVID-19 vaccine readiness as reported by parents for both themselves and their children.
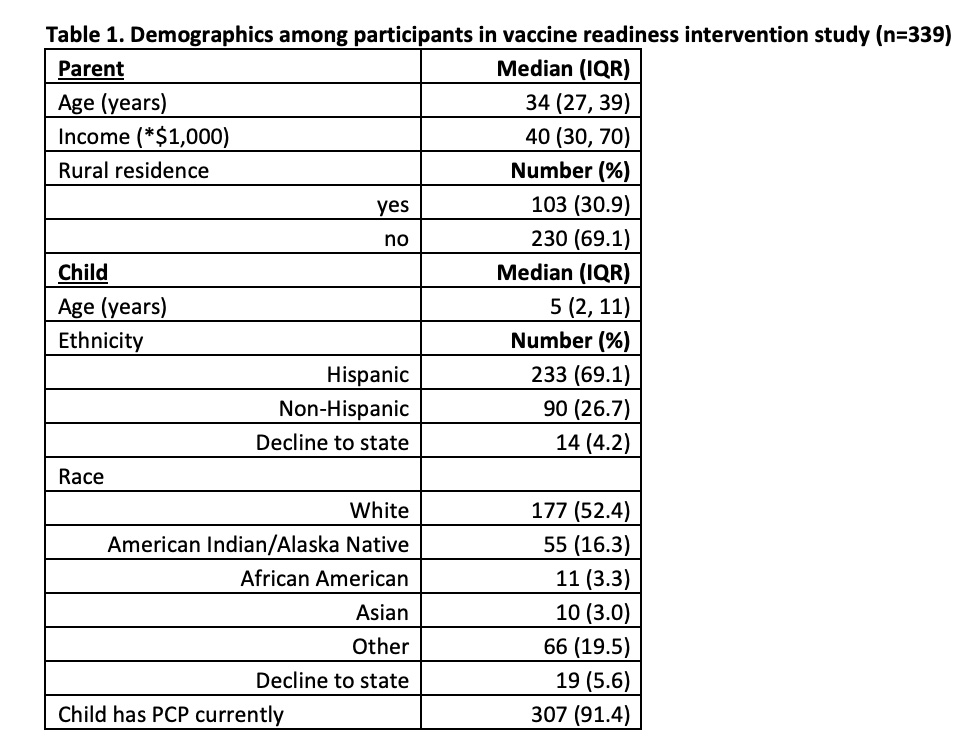
Design/Methods: The study consisted of a convenience sample of 339 parents accompanying pediatric patients to a university-based PED over a five-month period. Participants completed a pre-intervention survey via iPad that gathered standard descriptive data as well as data on COVID-19 beliefs and nine questions about general vaccine attitudes and readiness. Participants watched a novel 4-minute educational video created by the study team addressing risks and benefits of COVID-19 immunization and vaccinations overall. Subjects were then re-surveyed with only the nine questions about vaccine attitudes and vaccine readiness. Pre-/post-intervention attitude changes were measured using the nonparametric equivalent of the paired t-test, the Wilcoxon signed-rank test, and an alpha threshold of 0.05 was considered significant.
Results: Participant demographics are presented in Table 1 and beliefs about COVID-19 immunization are shown in Table 2. Table 3 shows pre-/post-intentions that changed significantly after the educational intervention. Post-intervention, COVID-19 vaccine acceptability as reported by parents increased for both themselves (p=0.0017) and their children (p=0.0038). Participants were also more likely to be willing to talk to a pediatric emergency medicine doctor about influenza vaccine administration for their children after the intervention (p=0.012).
Conclusion(s): A brief, inexpensive, video-based intervention in a PED targeted for parents is associated with improvement in vaccine readiness as reported by parents for both themselves and their children. This type of intervention should be further studied in both PEDs and in general pediatrics settings, with a goal toward improved vaccine uptake.
.jpg)
.jpg)
